PULSE
(lat. pulsus blow, push) - periodic fluctuations in the volume of blood vessels associated with the dynamics of their blood filling and pressure in them during one cardiac cycle.
Palpation and examination can normally detect the Pulse in all large arteries (arterial Pulse), and in some cases, the pulsation of the jugular veins is visually detected, i.e., the venous Pulse, which is usually necessary to detect and differentiate it from transmission oscillations of the arterial Pulse special research methods.
In rare cases, under special physiological conditions in practically healthy individuals, as well as in some forms of pathology, arteriolar, or so-called, is detected. precapillary pulse (syn. capillary pulse). The main part of the teaching about the Pulse, its origin and clinical significance relates to the arterial pulse.
The doctrine of P. arose in ancient times. Doctors of Ancient Greece, the Arab East, India, and China, studying the various properties of P., tried to make a diagnosis based on it, determine the prognosis of the disease and even the fate of a person. Hippocrates (5th-4th centuries BC) gave a description of the main types of pulse. K. Galen (2nd century AD), who devoted seven of his books to the doctrine of P., distinguished 27 types of P., many of its names have survived to the present day. Paracelsus (15th-16th centuries) proposed studying P. on both arms and legs, vessels of the neck, in the temples, and in the armpits. The discovery of blood circulation by W. Harvey (1628) laid the scientific foundations for the doctrine of P., which was significantly enriched in the mid-19th century. after the introduction of sphygmography studies into practice (see). Despite the diversified development of methods for studying the circulatory system, P.’s study and graphic methods of its registration retain their diagnostic value.
Basic characteristics of pulse
What are the main parameters of this indicator of the cardiovascular system that a doctor is interested in? Experts identify six main characteristics of the pulse:
1. Rhythm - alternating oscillations of the artery walls at regular intervals. Normally, the pulse is rhythmic and the intervals of successive beats are almost equal. However, with various pathologies, this indicator is disrupted and arrhythmia occurs (that is, alternating oscillations of the arterial walls occur at different time intervals).
2. Frequency – displays the number of oscillations of arterial walls occurring in one minute. The pulse may be rare, moderate or frequent. The normal heart rate indicators depend on many factors, and the norm is estimated based on the patient’s age. In some pathologies of the heart or blood vessels, the heart rate and pulse rate may not coincide (for example, in cases where the heart chambers are not completely filled with blood).
3. Filling - reflects the volume of blood released into the arteries from the heart chambers. Normally, the lumen of the artery fills completely and vibrations of the vascular walls become more noticeable - this indicator is characterized as “full pulse”. If the pulse is difficult to palpate, the doctor characterizes it as “empty.”
4. Tension - determined by the force of pressure on the artery, which is necessary to completely stop the flow of blood in the lumen of the artery. This indicator depends on the level of systolic pressure. With hypertension, the pulse becomes hard (or tense) and effort is required to compress the artery, and a soft pulse is said to be in cases where this action is performed without much effort.
5. Size – depends on filling and voltage. It is determined by the degree of oscillation of arterial walls between contraction and relaxation, as well as the elasticity of blood vessels. There are several types of heart rate. A small pulse is provoked by narrowing of the aorta, excessive elasticity of the vascular walls or cardiac tachycardia. Large - occurs in cases where the heart pumps a larger volume of blood through overstrained blood vessels (for example, with overproduction of thyroid hormones or aortic valve defects). Intermittent - caused by severe damage to the heart muscle and appears when large and small waves alternate. A thread-like pulse is characterized by weak palpation of beats and occurs during massive bleeding or shock.
6. Shape - determined only instrumentally and reflects the rate of change in the volume of the arterial lumen when the vessel is filled with blood. When assessing this pulse parameter, the doctor can characterize it as slow, fast or dicrotic.
Test with answers on “Nursing” Part 2
Test tasks “Nursing” were developed by teachers based on the National Standards of the Russian Federation “Technologies for performing simple medical services”, and are intended for independent preparation of students for certification testing. These test tasks are designed in such a way that you need to choose one correct answer out of five proposed ones.
204. Pulse rate during bradycardia
1) less than 40 beats per minute; 2) less than 45 beats per minute; 3) less than 50 beats per minute; 4) less than 55 beats per minute; 5) less than 60 beats per minute.
205. Indicate the normal pulse rate of an adult patient in one minute
1) 40 — 50; 2) 60 — 80; 3) 70 — 90; 4) 50 — 70; 5) 90 — 100.
206. If the pulse of a seriously ill patient is not detected on the radial artery, then the nurse must try to determine it on the artery
1) dorsum of the foot; 2) popliteal; 3) sleepy; 4) temporal; 5) elbow.
207. Pulse voltage depends
1) on the value of cardiac output; 2) from blood pressure; 3) from the total amount of circulating blood; 4) from heart rate; 5) on the patient’s age.
208. Which fingers are used to palpate the pulsating radial artery when examining the pulse?
1) first finger; 2) first and second; 3) second and third; 4) second, third, fourth; 5) second, third, fourth and fifth.
209. Select one of the pulse properties
1) voltage; 2) hypotension; 3) tachypnea; 4) atony; 5) dystonia.
210. Determine what does not belong to the properties of the pulse
1) depth; 2) frequency; 3) rhythm; 4) filling; 5) tension.
211. The size of the pulse varies
1) big; 2) complete; 3) empty; 4) hard; 5) soft.
212. Pulse deficiency occurs when
1) tachycardia; 2) decrease in blood pressure; 3) atrial fibrillation; 4) increased blood pressure; 5) bradycardia.
213. By filling the pulse is distinguished
1) rhythmic, arrhythmic; 2) fast, slow; 3) full, empty; 4) hard, soft; 5) correct, incorrect.
214. The most interconnected properties of the pulse
1) tension and filling; 2) tension and rhythm; 3) frequency and rhythm; 4) speed and frequency; 5) filling and rhythm.
215. The rhythmic pulse of an adult patient is determined
1) in one minute; 2) in 30 seconds, multiplying the result by two; 3) in 15 seconds, multiplying the result by four; 4) in 10 seconds, multiplying the result by six; 5) in 6 seconds, multiplying the result by ten.
216. An arrhythmic pulse in an adult patient is determined
1) in one minute; 2) in 30 seconds, multiplying the result by two; 3) in 15 seconds, multiplying the result by four; 4) in 10 seconds, multiplying the result by six; 5) in 6 seconds, multiplying the result by ten.
217. The pulse is distinguished by voltage
1) rhythmic, arrhythmic; 2) fast, slow; 3) full, empty; 4) hard, soft; 5) tonic, atonic.
218. All places for detecting pulse except
1) carotid artery; 2) temporal artery; 3) radial artery; 4) abdominal aorta; 5) arteries of the dorsum of the foot.
219. What condition must be met before standard blood pressure measurement?
1) 1-2 hours after eating; 2) 1 hour after smoking; 3) 1 hour after drinking coffee; 4) 2 hours after water procedures; 5) all of the above.
220. When measuring blood pressure, the nurse heard the appearance of Korotkoff sounds (systolic pressure), but could not determine diastolic pressure. What is the reason?
1) too little air in the cuff; 2) the head of the phonendoscope is pressed too tightly to the brachial artery; 3) too much air in the cuff; 4) the cuff is released too quickly; 5) discrepancy between the size of the cuff and the circumference of the shoulder.
221. Standard blood pressure measurement is carried out
1) 1-2 hours after eating; 2) 1 hour after smoking; 3) 1 hour after drinking coffee; 4) after a 10 minute rest; 5) all of the above are true.
222. Blood pressure is measured
1) only sitting and lying down; 2) only lying down; 3) sitting, lying, standing; 4) standing only; 5) there is no correct answer.
223. The difference between systolic and diastolic blood pressure is called
1) maximum blood pressure; 2) minimum blood pressure; 3) pulse pressure; 4) pulse deficiency; 5) working pressure.
224. What indicator of blood pressure can we judge when Korotkoff sounds disappear over the brachial artery?
1) pulse pressure; 2) diastolic pressure; 3) systolic pressure; 4) blood pressure; 5) working pressure.
225. What blood pressure indicator can we judge when Korotkoff sounds appear over the brachial artery?
1) pulse; 2) diastolic; 3) systolic; 4) arterial; 5) working.
226. What equipment is used to measure blood pressure?
1) tonometer; 2) thermometer; 3) dynamometer; 4) spirometer; 5) phonendoscope.
227. What device is used to listen to sounds on the brachial artery when measuring blood pressure?
1) palpated with fingers; 2) phonendoscope; 3) tonometer; 4) peak flow meter; 5) thermometer.
228. Choose the correct statement. The blood pressure cuff must be secured
1) so that not a single finger passes between the cuff and the shoulder; 2) so that 2 fingers pass between the cuff and the shoulder; 3) so that 1 finger passes between the cuff and the shoulder; 4) the cuff should fit tightly around the shoulder; 5) doesn't matter.
229. What is the correct position of the patient’s hand when measuring blood pressure?
1) bent at the elbow joint, palm up; 2) bent at the elbow joint, palm down; 3) extended at the elbow joint with the palm down; 4) extended at the elbow joint with the palm up; 5) the hand is lowered down.
230. During the patient’s first visit, it is necessary to measure blood pressure
1) 1 time on one hand; 2) 2 times on one hand; 3) 3 times on one hand; 4) 1 time on both hands; 5) 3 times on both hands.
231. The parameters that determine the value of blood pressure include
1) the strength of heart contractions; 2) heart rate; 3) tone of the arterial wall; 4) from physical activity; 5) patient's age.
232. Normal figures for systolic blood pressure according to WHO classification (mmHg)
1) 120 — 130; 2) 120 — 129; 3) 100 — 110; 4) 70 — 80; 5) 40 — 50.
233. Normal figures for diastolic blood pressure according to WHO classification (mmHg)
1) 120 — 130; 2) 110 — 120; 3) 100 — 110; 4) 80 — 84; 5) 40 — 50.
234. A patient's blood pressure is 150/100 mmHg. What is the name of the condition?
1) hyperthermia; 2) arrhythmia; 3) hypertension; 4) hypotension; 5) normotension.
235. A patient's blood pressure is 80/50 mmHg. What is the name of the condition?
1) hyperthermia; 2) arrhythmia; 3) hypertension; 4) hypotension; 5) normotension.
236. The respiratory rate in an adult patient is determined
1) in one minute; 2) in 30 seconds, multiplying the result by two; 3) in 15 seconds, multiplying the result by four; 4) in 10 seconds, multiplying the result by six; 5) in 6 seconds, multiplying the result by ten;
237. The nature of shortness of breath is
1) inspiratory; 2) expiratory; 3) mixed; 4) physiological; 5) all of the above are true.
238. Shortness of breath with difficulty inhaling is called
1) mixed; 2) periodic breathing; 3) inspiratory; 4) expiratory; 5) pathological.
239. Inspiratory dyspnea is characterized by
1) difficulty in inhaling; 2) cough with a lot of foamy sputum; 3) difficulty in exhaling; 4) difficulty in inhaling and exhaling; 5) cough with difficult to clear sputum.
240. Shortness of breath with difficulty exhaling is called
1) mixed; 2) periodic breathing; 3) inspiratory; 4) expiratory; 5) pathological.
241. Expiratory dyspnea is characterized by
1) difficulty in inhaling; 2) cough with a lot of foamy sputum; 3) difficulty in exhaling; 4) difficulty in inhaling and exhaling; 5) cough with difficult to clear sputum.
242. What is the normal respiratory rate of an adult patient in one minute?
1) 30-36; 2) 24-28; 3) 20-24; 4) 16-20; 5) 10-16.
243. When calculating the frequency of respiratory movements, only the quantity is taken into account
1) breaths; 2) exhalations; 3) inhalation delays; 4) delays in exhalation.
244. When collecting urine to determine daily diuresis
1) collect urine for any 24 hours; 2) collect urine from the moment the patient wakes up until eight in the morning the next day; 3) at eight o’clock in the morning the patient urinates in the toilet, then until eight o’clock the next morning all urine is collected in a container; 4) collect urine every three hours, eight portions in total; 5) collect urine for 12 hours, multiply the resulting volume by two.
245. Pleural puncture is performed for the purpose of
1) separation of pleural adhesions; 2) suction of sputum from the bronchi; 3) reduction of pain; 4) removal of fluid from the pleural cavity; 5) removal of a foreign body from the pleural cavity.
246. Acrocyanosis is cyanosis
1) lips; 2) lips and tip of the nose; 3) lips and tip of the nose, fingers; 4) lips and tip of the nose, fingers and toes; 5) lips and tip of the nose, fingers and toes, ears.
247. Accumulation of fluid in the abdominal cavity is
1) anasarca; 2) hydrothorax; 3) ascites; 4) hydropericarditis; 5) pastiness.
248. Widespread swelling of the subcutaneous tissue throughout the body is
1) ascites; 2) hydropericarditis; 3) anasarca; 4) hydrothorax; 5) pastiness.
249. The nurse can determine the presence of external edema in a patient using
1) weighing; 2) palpation of the legs; 3) measurements of daily diuresis; 4) general examination of appearance; 5) palpation of the hands.
250. When determining body weight, all conditions must be met, except
1) on an empty stomach; 2) after emptying the bladder; 3) after bowel movement; 4) in the same clothes; 5) after water procedures.
251. Accumulation of fluid in the pleural cavity is
1) anasarca; 2) hydrothorax; 3) ascites; 4) hydropericarditis; 5) pastiness.
252. What is the name of the relationship between daily diuresis and fluid introduced into the body per day?
1) daily diuresis; 2) water balance; 3) dysuria; 4) oliguria; 5) body mass index.
253. Anthropometry includes the measurement of all of the following parameters, except
1) growth; 2) weight; 3) strength; 4) chest circumference; 5) head circumference.
254. The following indicators are recorded in the temperature sheet
1) graphical representation of temperature; 2) graphical representation of respiratory rate; 3) graphic representation of body weight; 4) graphical representation of blood pressure; 5) all of the above.
255. With low-grade fever, body temperature rises to digits
1) 37.5°C; 2) 38°C; 3) 38.5°C; 4) 39°C; 5) 37°C.
256. Indicate in what period of fever the patient is advised to use physical cooling methods
1) during a period of rising temperature; 2) during the period when the temperature is at high levels; 3) during the period of lytic temperature drop; 4) during a period of critical temperature drop; 5) doesn't matter.
257. Specify dependent nursing intervention for acute febrile conditions
1) change of underwear and bed linen; 2) drink plenty of fluids; 3) use of an ice pack; 4) use of a heating pad; 5) parenteral administration of antipyretics.
258. With febrile fever, body temperature rises to
1) 38°C; 2) 39°C; 3) 40°C; 4) 41°C; 5) 37.5°C.
259. Determine which period of fever is typical for this patient’s condition - pallor, “goose bumps”, chills, muscle tremors, lack of sweating
1) for a critical decrease in body temperature; 2) for lytic reduction of body temperature; 3) for the stage of rising body temperature; 4) for the stage of body temperature standing at high levels; 5) when body temperature drops below normal.
260. Specify independent nursing intervention for lytic decrease in temperature
1) warming the patient; 2) change of underwear and bed linen; 3) use of an ice pack; 4) parenteral administration of antipyretics; 5) placing the patient in a position with the leg end raised.
261. Select what the nurse needs to do when caring for a patient in the first period of fever
1) disclose the patient; 2) give a cold drink; 3) apply cold to the head; 4) give a hot drink and cover the patient; 5) feed the patient.
262. Select what the nurse needs to do when caring for a patient in the second period of fever
1) give a hot drink; 2) put mustard plasters on the chest; 3) give plenty of cool drinks; 4) cover with heating pads; 5) cover with a blanket.
263. Choose what applies to physical cooling methods
1) hot foot baths; 2) warming compress; 3) warm drink; 4) cold compress on large vessels; 5) parenteral administration of antipyretics.
264. What first aid is needed when the temperature drops critically?
1) mustard plasters on the chest; 2) cold compress on the head; 3) plenty of cool drinks; 4) cover with heating pads, hot strong tea, coffee; 5) disclose the patient.
265. Indicate the condition that may occur with a critical decrease in body temperature
1) rhythm disturbance; 2) a sharp drop in blood pressure; 3) a sharp rise in blood pressure; 4) urination disorders; 5) abdominal pain.
266. Before measuring body temperature, the armpit should be
1) inspect and wipe dry; 2) wash with water and wipe; 3) wipe with alcohol; 4) just inspect; 5) wipe with any skin antiseptic.
267. During a period of critical temperature drop, it is necessary
1) raise the foot end of the bed; 2) cover with heating pads and cover the patient; 3) give strong sweet tea or coffee; 4) control of pulse and blood pressure; 5) all of the above are true.
268. Body temperature rises during hyperpyretic fever
1) above 41°C; 2) 40 - 41°C; 3) 39 - 40°C; 4) 38 - 39°C; 5) 37 - 38°C.
269. Normally, a person’s body temperature changes during the day by
1) 1 - 1.5°C; 2) 0.8 - 1°C; 3) 0.5 - 0.8°C; 4) 0.3 - 0.8°C; 5) 0.1 - 0.3°C.
270. Indicate the frequency of measurements of the patient’s body temperature in the hospital during the day
1) 4 times a day; 2) 3 times a day; 3) 2 times a day; 4) once a day; 5) as much as necessary.
271. Maximum (lethal) body temperature at which death occurs
1) 40.5°C; 2) 41°C; 3) 41.5°C; 4) 42°C; 5) 42.5°C.
272. The following number of periods are distinguished in the development of fever
1) five periods; 2) four periods; 3) three periods; 4) two periods; 5) one period.
273. By how many beats per minute does the pulse rate increase when body temperature increases by 1°C (in beats)
1) 20; 2) 15; 3) 10; 4) 5; 5) 2.
274. Determine which period of fever is typical for this patient’s condition - severe weakness, profuse cold sweat, pale skin, thready pulse and decreased blood pressure
1) for the first period of fever; 2) for lytic temperature reduction; 3) for a critical decrease in temperature; 4) for the second period of fever; 5) this condition can occur in any period of fever.
275. The patient’s physiological body temperature is often lower
1) in the morning; 2) at lunch; 3) in the evening; 4) at night; 5) does not change during the day.
276. Select the time to measure the temperature in the armpit with a mercury thermometer
1) 10 minutes; 2) 5 minutes; 3) 7 minutes; 4) 15 minutes; 5) 20 minutes.
Article Rating
Heart rate table by age
Normal heart rate depends on many factors: age, gender, activity (physical or emotional) or rest, level of physical fitness or the presence of diseases. Pulse rate is measured in beats per minute, and the rate of this indicator is determined by age.
Normal heart rate values for children:
| Child's age | max and min indicators | Average value |
| 0 – 1 month | 110 – 170 | 140 |
| 1 – 12 months | 102 – 162 | 132 |
| 1 – 2 years | 94 – 155 | 124 |
| 4 – 6 years | 86 – 126 | 106 |
| 6 – 8 years | 78 — 118 | 98 |
| 8 – 10 years | 68 – 108 | 88 |
| 10 – 12 years | 60 – 100 | 80 |
| 12 – 15 years | 55 – 95 | 75 |
Normal heart rates for adults:
| Age | max and min indicators | Average value |
| Up to 50 years | 60 – 80 | 70 |
| 50 – 60 years | 65 – 85 | 75 |
| 60 – 80 years | 70 – 90 | 80 |
What is the pulse like?
Experts distinguish the following types of pulse:
- arterial - has the greatest diagnostic value, occurs as a result of rhythmic jerk-like oscillations of the arterial walls when their blood supply changes during heart activity, is characterized by rhythm, frequency, filling, tension, height and shape (or speed);
- capillary (or Quincke's pulse) - detection of such a pulse is not the norm, since in healthy people the blood flow in the capillaries is continuous due to the work of the precapillary sphincters, such a pulse is determined by the intensity of the color of the nail bed, the skin of the forehead rubbed with the fingers and the lower lip pressed under the cover glass;
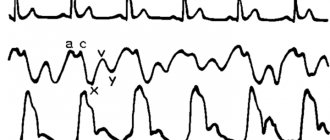
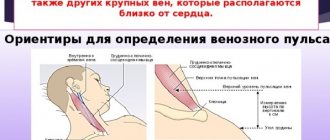
- venous - expressed in the pulsation of the cervical jugular veins and other large venous vessels located near the heart; it is rarely present in the peripheral veins; according to the sphygmogram and venogram, it can be characterized as negative or positive.
Video: Pulse. What does his silence say?
Definition
In the general concept of this term there is a division into types of pulse. Each of them has its own normative values, which show the functioning of the entire organism.
Arterial
This is a rhythmic contraction of the walls of the arteries during the release of blood supplied by the contracting heart muscle. Pulse waves begin at the mouth of the aortic valve as the left ventricle of the heart ejects blood.
Its main wave is formed due to a surge in systolic pressure when the vascular bed expands, and when it declines, the walls take their original shape. Cyclic contractions of the myocardium create a rhythm of oscillation of the aortic surfaces, which leads to a mechanical pulse wave.
It passes first through large arteries, smoothly moving to small ones, and lastly to the capillaries.
The further the vasculature is from the heart, the smaller the blood pressure and pulse pressure waves will be.
Capillary
It is also called Quincke's pulse. This is the movement of capillaries, which is most often tested by pressing on the tip of the nail. Redness of the nail plate shows heart rate. Its manifestation is a deviation from the norm, because in a healthy person, the movement of blood through the capillary network should be continuous, since the precapillary sphincters work constantly.
Venous
The heartbeat is reflected not only in the arterial bed, but also in the venous bed. If the venous pulse is positive, tricuspid valve insufficiency is diagnosed. But negative is considered to be normative, but it is not present in the small and medium venous network.
If we compare venous waves with arterial ones, then the first ones are smoother, even sluggish, with a longer period of rise than fall.
Why measure your pulse?
Pulse is one of the important parameters of the quality of physiological processes, reflecting the state of health, level of physical fitness or the presence of diseases of the heart, blood vessels and other systems and organs. The indicators given in the tables above are the normal heart rate for healthy people at rest. It should be remembered that any changes in the body can provoke deviations from the norm in different directions. For example, during pregnancy or menopause, hormonal changes occur that can affect the pulse rate. A person's heart rate can change under the influence of many factors.
Rapid pulse - tachycardia - can occur in the following physiological conditions or pathologies:
- emotional outburst or stressful situation;
- pregnancy;
- menopause;
- hot weather or stuffy room;
- overwork;
- high level of physical fitness;
- consumption of products containing caffeine;
- taking certain medications;
- heavy menstrual bleeding;
- severe pain;
- diseases of the endocrine and nervous system, blood vessels and heart, high temperature in some infections, neoplasms, anemia, bleeding, etc.
Physiological or pathological slowing of the pulse - bradycardia - can be provoked by the following factors:
- dream;
- high fitness of the heart muscle (in athletes, active people);
- age-related changes;
- intoxication;
- increased intracranial pressure;
- myocardial infarction;
- inflammatory processes in the tissues of the heart;
- organic heart lesions;
- peptic ulcer;
- hypothyroidism;
- taking certain medications.
Varieties of PS
Definition area of capillary PS
Since the circulatory system is represented by arteries, veins and capillaries, there are the following types of pulse in humans:
- arterial - central (on the aorta and carotid artery) and peripheral (on the arteries of the extremities);
- venous - on the walls of large veins that are located near the heart.
- capillary – true and precapillary.
Among the many types of PS palpable in the arteries, it is worth highlighting the carotid pulse. It is palpated in the area of the carotid artery. In this case, it is better to lie down or sit, since excessive pressure can cause the heart to slow down or even stop.
High and/or galloping carotid PS may be a sign of hypertension, aortic insufficiency, aortic duct nonunion, and other hypermetabolic conditions that can cause a rapid rise and fall in blood pressure.
What is capillary pulse?
The smallest blood vessel, the capillary, consists of arterial and venous branches, and an geniculate bridge between them. The true capillary pulse is the pulsation of the arterial branch of the capillary. It appears in the nail bed when pressure is applied to the end of the nail phalanx and appears as a pulsating discoloration (see photo above).
True capillary pulse appears without pressure in two cases:
- in young people after overheating in the sun or in a bath;
- in patients diagnosed with Thyrotoxicosis (thyroid hyperfunction).
Blood arteries larger than capillaries are called arterioles and venules. Precapillary or capillary Quincke's pulse is a beating of the arterioles, which is caused by insufficiency of the aortic valve.
You can see such a pulsation - a change in the color of the skin that matches the heart rate and PS - in the forehead or on the lower lip, as well as in the bed of the nail plates (without pressing on them).
What are the types of rhythm disturbances?
Normally, contractions of the heart muscle are caused by the occurrence of electrical impulses emanating from the sinus node (the main pacemaker of the heart rhythm). All contractions occur constantly and rhythmically, that is, at almost the same interval of time. And disturbances in the rhythm of the pulse, caused by incorrectly received electrical impulses, are called arrhythmia. In such cases, the pulse becomes too slow, fast, irregular or irregular.
Both functional disorders and diseases can provoke arrhythmias. Typically, the root causes of such a deviation are:
- disruption of impulse conduction through one of the nodes of the conduction system of the heart;
- changes in the formation of an impulse in one of the nodes.
Depending on the origin, arrhythmias are as follows:
| By source of occurrence |
|
| By number of sources of rhythm disturbance |
|
| According to the nature of the disturbance in the conduction of electrical impulses |
|
With changes in the occurrence of an impulse in the sinus node, the following types of arrhythmias develop:
- sinus bradycardia (55 or less beats per minute) - provoked by heart pathologies, arterial hypotension or hypothyroidism, accompanied by dizziness, feelings of general weakness and discomfort;
- sinus tachycardia (more than 90 beats per minute) - caused by strong emotional outbursts, physical exertion, fever and, sometimes, heart pathologies, accompanied by a feeling of palpitations;
- sinus arrhythmia (irregular alternation of heart beats) – often detected in adolescents and children and associated with breathing (the heart rate increases as you inhale and decreases as you exhale), usually does not require treatment;
- sick sinus syndrome (expressed in bradycardia or bradyarrhythmia with paroxysms of extrasystole and atrial fibrillation) - provoked by injuries and abnormalities in the functioning of the heart, disturbances in the functioning of the autonomic nervous system or the intake of toxic substances and drugs, occurs latently or causes weakness, fainting and palpitations .
If myocardial cells lose the ability to generate an electrical impulse into an action potential, then a person develops the following types of arrhythmias:
- extrasystole (extraordinary or premature contractions of the heart muscle, an extra heartbeat) - provoked by intense emotions, autonomic dysfunction, abuse of nicotine, caffeine and alcohol or organic pathologies of the heart, manifested in the form of pulsation in the epigastric region, pallor, increased sweating, sensations of lack of oxygen and strong tremors and fading of the heart, fainting;
- paroxysmal tachycardia (pulse rate 140 - 240 beats per minute) - attacks appear and disappear suddenly, last from several seconds to several hours, are provoked by hypertension, heart pathologies, pneumonia, sepsis, taking medications (Quinidine, cardiac glycosides, diuretics and Ephedrine) or diphtheria, are accompanied by sensations of palpitations, weakness and the presence of a lump in the throat, frequent urination and increased sweating.
The most dangerous type of heart rhythm disorder is atrial fibrillation. As a result of this deviation from the norm, a person may develop thromboembolism, cardiac arrest and heart failure. During this disorder, a person experiences chest pain, increased heart rate, ischemia of the heart muscle (up to a heart attack), signs of atrial fibrillation on the ECG and heart failure. The following factors can provoke the development of atrial fibrillation:
- heart disease;
- stroke;
- severe stress;
- taking high doses of ethanol;
- overdose of certain medications;
- surgery.
Causes of weak pulse filling
Depending on changes in this indicator, the following types of pulse are distinguished:
- Full. This means that the blood supply to the arteries is sufficient.
- Empty. Such a pulse occurs when the volume of blood ejected by the heart during systole is small. The causes of this condition may be heart pathology (heart failure, arrhythmias with too high heart rate) or a decrease in blood volume in the body (blood loss, dehydration).
A full pulse is observed with an increase in stroke volume of the heart and/or with an increase in circulating blood volume.
In a healthy person, it can be recorded during physical activity. The higher the training, the more efficiently the heart contracts. This determines the limit to which an increase in heart rate is accompanied by an increase in stroke volume. For example, with a heart rate of 150 per minute, its filling will be different for an athlete and an untrained elderly person.
Also, a well-filled pulse is characteristic of physiological erythrocytosis, that is, an increase in the number of red blood cells in the blood. This is mainly typical for residents of mountainous areas.
Pathological conditions and diseases accompanied by increased pulse filling:
- arterial hypertension, especially in the early stages of development;
- hyperthyroidism, that is, excessive hormonal activity of the thyroid gland;
- a significant volume of intravenous infusions exceeding the needs of the body;
- respiratory failure due to lung diseases;
- chronic poisoning with copper, phosphorus, manganese, cobalt;
- Erythremia is a bone marrow tumor accompanied by the production of excess red blood cells.
https://www.youtube.com/watch?v=ytaboutru
A weak pulse is recorded in diseases accompanied by a decrease in cardiac output or a decrease in circulating blood volume. Possible reasons:
- acute heart failure due to myocardial infarction complicated by hypertensive crisis;
- paroxysmal tachycardia – supraventricular and ventricular;
- tachysystolic form of atrial fibrillation, or atrial fibrillation;
- ventricular fibrillation and flutter – life-threatening arrhythmia;
- chronic heart failure of functional class III - IV, accompanied by a deterioration in the systolic function of the myocardium, that is, a decrease in its contractility;
- dehydration caused by intense sweating and insufficient water intake into the body (working at high ambient temperatures);
- acute vascular insufficiency that occurs with any type of shock - anaphylactic (allergic), hemorrhagic (with rapid blood loss), traumatic, painful, etc.;
- arterial hypotension - decreased blood pressure due to hypothyroidism, adrenal insufficiency;
- anemia resulting from acute blood loss after injury, surgery, bleeding;
- diabetes insipidus, in which up to 10–12 liters of fluid per day are lost in the urine;
- decompensation of diabetes mellitus, accompanied by a significant amount of urine excreted;
- severe renal failure;
- significant burns;
- diseases accompanied by repeated vomiting and/or prolonged intense diarrhea, for example, cholera and other intestinal infections.
A weak, thread-like or empty pulse is of greater clinical significance, as it is caused by a significant impairment of myocardial contractility or severe disturbances in the vascular bed. Such conditions are accompanied by oxygen starvation of the brain, kidneys, and heart and require emergency medical care.
Author of the article: Active cardiologist V. O. Chubeiko. Higher medical education (Omsk State Medical University with honors, awarded the academic degree of Candidate of Medical Sciences).
Heart rate
Heart rate is the number of heart contractions per unit of time. It reflects the frequency of contractions of the ventricles of the heart in one minute and normally ranges from 60 to 80 beats (in an adult and healthy person). This indicator is often confused with the pulse, while this parameter of the cardiovascular system displays the number of oscillations of the vessel walls in response to heart contractions. Typically, both heart rate and pulse are approximately the same.
What does heart rate depend on?
Pulse characteristics may vary depending on various factors such as environment, age, physiological or pathological reasons. The gender of a person is also important, as a woman’s heart beats at a higher speed than a man’s. To summarize, heart rate largely depends on the reasons:
- Physiological, such as load, stress, food consumption and digestion. There are drinks that have a significant effect on the pulse. These are caffeine-containing products, including Coca-Cola and alcohol. Smokers also have a faster heart rate. Sleep and monotonous work help slow down the process of ventricular fibrillation and the ejection of blood.
- Pathological, for example, infectious diseases, hypertension, neoplasms, asthma, bronchitis, heart attack, large blood loss. Often the cause of a slow heart rate is a side effect of certain medications. If the heart is malfunctioning, then the pulse waves will be irregular, and if the veins in the arms and legs are blocked, they will be completely absent.
Pulse form
The shape of the pulse reflects the rate of change in pressure between contraction and relaxation of the heart muscle. Depending on these indicators, doctors distinguish the following forms of pulse fluctuations:
- rapid pulse - is a sign of aortic insufficiency or thyrotoxicosis, occurs due to the fact that a lot of blood is pushed out of the ventricles and the pressure during diastole decreases sharply;
- slow pulse - occurs with mitral regurgitation or narrowing of the aortic walls, manifested by small pressure drops;
- dicrotic pulse - appears when the tone of peripheral vessels deteriorates and is manifested by the passage of an additional wave of oscillations through the vessels.
Voltage
Depending on changes in this indicator, the pulse also changes. The characteristics of the pulse according to its voltage include division into the following types:
- Firm pulse. Caused by high blood pressure (BP), primarily systolic. In this case, it is very difficult to squeeze the artery with your fingers. The appearance of this type of pulse indicates the need for urgent correction of blood pressure with antihypertensive drugs.
- Soft pulse. The artery contracts easily, and this is not very good, because this type of pulse indicates that the blood pressure is too low. It can be due to various reasons: a decrease in the volume of circulating blood, a decrease in vascular tone, and ineffective heart contractions.
How to properly examine the pulse?
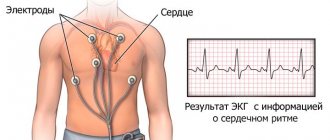
The arterial pulse is most easily measured with a finger, while the venous and capillary pulse cannot be determined by palpation and are measured using special techniques. In some cases, to study the arterial pulse, the patient is prescribed the following instrumental methods:
- sphymography;
- sphygmomanometry;
- ECG or Holter ECG;
- Pulse symmetry.
Pulse counting can be done by yourself, a loved one, or a doctor. Remember, the person who is taking the pulse must be relaxed and emotionally calm, his hand must be in a comfortable position!
Video: How to measure pulse
Most often, the measurement is performed by palpating the radial artery at the wrist. To do this, press the artery with two or four fingers so that the fingertips feel the vibrations of the arterial walls. After this, they note the time (it is better to do this with a stopwatch) and begin to count the pulse. The number of vibrations of the arterial walls can be calculated in 1 minute, and if the pulse is rhythmic, then the measurement can be accelerated by counting the frequency of beats in 30 seconds and multiplying the result by 2.
Sometimes the pulse is measured in other arteries:
- ulnar - on the bend of the elbow or in the center of the wrist;
- carotid - on the neck on the side of the thyroid cartilage and closer to the chin;
- axillary - at the level of the edge of the first rib;
- femoral - on the inner side of the thigh (closer to the pubic symphysis);
- temporal - on the temple just above the cheekbone.
Treatment if the pulse on the wrist is difficult to feel
To treat the most common causes of poor palpation of the pulse on the wrist, use:
- atherosclerosis: cholesterol-lowering drugs (Atorvastatin, Roxera) that reduce blood viscosity (Curantil, Aspirin);
- scalene muscle syndrome: muscle relaxants (Sirdalud, Mydocalm), B vitamins (Kombilipen), massage, exercise therapy;
- heart failure: cardiac glycosides (Digoxin), which improve metabolism in the myocardium (Riboxin, Mildronate);
- arterial hypotension, neurocirculatory dystonia of the hypotonic type: ginseng tincture, hydromassage, circular shower, electrophoresis;
- arterial spasm due to smoking: Trental, Dipyridamole, quitting cigarettes;
- anemia: iron supplements (Sorbifer Durules), vitamins (Milgamma, Vitrum);
- decreased thyroid function: Iodomarin, L-thyroxine.
The pulse cannot be felt in the arm due to low blood pressure, weakened arterial tone, and impaired peripheral circulation. If it is on one hand, then the cause should be sought in unilateral compression due to osteochondrosis, carpal tunnel syndrome, congenital anomaly of the subclavian artery.