All about plasma
Plasma is a liquid formed by water and dry substances. It makes up the bulk of the blood - about 60%. Thanks to plasma, blood has a liquid state. Although according to physical indicators (density) plasma is heavier than water.
Macroscopically, plasma is a transparent (sometimes cloudy) homogeneous liquid of light yellow color. It collects in the upper part of the vessels when the formed elements settle. Histological analysis shows that plasma is the intercellular substance of the liquid part of the blood.
Plasma becomes cloudy after a person consumes fatty foods.
Diseases affecting the properties of plasma and issues of their therapy
The liquid part of the blood is extremely sensitive to changes in the concentration of active substances. There is a group of pathologies that can provoke disturbances in the functioning of the body.
Congenital anomalies, coagulopathies
This includes hemophilia as a classic type of disorder. It is accompanied by a decrease in the production of fibrinogen and other coagulation factors. Any deviations require urgent treatment. Especially if problems with clotting begin.
Therapy. It is carried out when there is a reason for it. Minor fluctuations are quite common and do not indicate the development of a pathological process. At least not always. You need to be wary if the indicator has dropped significantly or a group of levels has been violated.
Depending on the condition, homeostatic drugs are used. They stop the bleeding.
Regular transfusions of red blood cells and plasma are also prescribed. Everything is determined by the severity of the disease.
With congenital forms of coagulopathies, you can only relieve the symptoms. In other cases, it is necessary to correct the main diagnosis. The one that led to the violation.
Thrombocytopathies
They occur in approximately 3-4% of cases of the total number of blood diseases. The disorder is accompanied by a decrease in the functional activity of formed cells. However, their number remains at a normal level.
Thrombocytopathy is accompanied by coagulation disorders. The disease is practically never primary, so you need to look for the main cause and work with it.
Treatment. It is carried out under the supervision of a hematologist. Special medications such as glucocorticoids are prescribed.
In some cases, surgery to resect the spleen is practiced. But this is rather an exception to the rule. The question of the appropriateness of such a measure is decided by the doctor after a complete diagnosis. At a minimum, they examine the blood and check the functioning of the liver.
Thrombocytopenia
The opposite phenomenon. In this condition, the functionality of the formed cells remains at a normal level. However, the number of cytological structures drops sharply.
The number of records drops to a critical level if nothing is done. Treatment depends on the underlying cause.
Therapy. As a rule, drug correction is carried out at an early stage. Glucocorticoid drugs are prescribed. Prednisolone and others.
The composition of human blood plasma does not change, but the concentration of many proteins decreases. These disorders are secondary, caused by insufficient functioning of formed cells. This influence is suppressed when treatment begins. It is important to take the necessary actions in a timely manner.
The second line is the actual operational correction. In almost 50% of patients, recovery is achieved through removal of the spleen. Although there are exceptions.
Read more about the causes of thrombocytopenia and treatment methods in this article.
Vitamin deficiencies
Different types. We are talking about disorders associated with insufficient intake of microelements. Chlorine, zinc and others.
Treatment is standard. It is necessary to correct the main diagnosis. Plus, vitamins and other substances are introduced at the initial stage. Artificial analogues from outside.
Anemia
Accompanied by hematopoietic disorders. A particularly common variant of the pathological process is the so-called iron deficiency anemia. It is associated with a deficiency of the microelement of the same name.
There are other types as well. Including vitamin profile. With a deficiency of B9, 12, a restructuring of hematopoiesis begins in an abnormal manner (megaloblastic anemia). Plasma also suffers.
Therapy. Artificial administration of iron supplements, treatment of the primary pathological process. One that affected the condition of liquid connective tissue.
Diabetes mellitus and other metabolic disorders
Treatment. This is done using insulin. Other disorders, for example, those caused by the hypothalamus, require systematic administration of nootropics. For example, Piracetam.
Allergic reactions
Substances involved are also immunoglobulins. The properties of the plasma change: the blood becomes clogged with histamine and prostaglandins.
Therapy. It is carried out using antihistamines. Especially the first and third generations. For example, such names as Pipolfen, Tavegil, Suprastin, Citrine and similar are suitable.
Disturbances affect both plasma proteins and microelements. Which ultimately leads to disruption of the functioning of the entire organism or its individual systems.
Composition and objectives of non-protein compounds in plasma
Plasma contains:
- Organic compounds based on nitrogen. Representatives: uric acid, bilirubin, creatine. An increase in the amount of nitrogen signals the development of azotomy. This condition occurs due to problems with the excretion of metabolic products in the urine or due to the active destruction of protein and the entry of large amounts of nitrogenous substances into the body. The latter case is typical for diabetes, fasting, and burns.
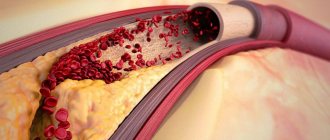
- Organic compounds that do not contain nitrogen. This includes cholesterol, glucose, lactic acid. Lipids also keep them company. All these components must be monitored, as they are necessary to maintain full functioning.
- Inorganic substances (Ca, Mg). Na and Cl ions are responsible for maintaining a constant pH of the blood. They also monitor osmotic pressure. Ca ions take part in muscle contraction and stimulate the sensitivity of nerve cells.
Blood plasma composition
Albumen
Albumin in plasma blood is the main component (more than 50%). It has a small molecular weight. The place of formation of this protein is the liver.
Purpose of albumin:
- Transports fatty acids, bilirubin, drugs, hormones.
- Takes part in metabolism and protein formation.
- Reserves amino acids.
- Forms oncotic pressure.
Doctors judge the condition of the liver by the amount of albumin. If the albumin content in plasma is reduced, this indicates the development of pathology. Low levels of this plasma protein in children increase the risk of developing jaundice.
Globulins
Globulins are represented by large molecular compounds. They are produced by the liver, spleen, and thymus.
There are several types of globulins:
- α – globulins. They interact with thyroxine and bilirubin, binding them. Catalyze the formation of proteins. Responsible for transporting hormones, vitamins, lipids.
- β – globulins. These proteins bind vitamins, Fe, and cholesterol. They transport Fe and Zn cations, steroid hormones, sterols, and phospholipids.
- γ – globulins. Antibodies or immunoglobulins bind histamine and take part in protective immune reactions. They are produced by the liver, lymph tissue, bone marrow and spleen.
There are 5 classes of γ-globulins:
- IgG (about 80% of all antibodies). It is characterized by high avidity (antibody to antigen ratio). Can penetrate the placental barrier.
- IgM is the first immunoglobulin that is formed in the unborn baby. The protein has high avidity. It is the first to be detected in the blood after vaccination.
- IgA.
- IgD.
- IgE.
Fibrinogen is a soluble plasma protein. It is synthesized by the liver. Under the influence of thrombin, the protein is converted into fibrin, an insoluble form of fibrinogen. Thanks to fibrin, a blood clot forms in places where the integrity of the vessels has been compromised.
Other proteins and functions
Minor fractions of plasma proteins after globulins and albumins:
- Prothrombin,
- Transferrin,
- immune proteins,
- C-reactive protein,
- Thyroxine binding globulin,
- Haptoglobin.
The tasks of these and other plasma proteins boil down to:
- Maintaining homeostasis and aggregative state of blood,
- Controlling immune reactions
- Transport of nutrients
- Activation of the blood clotting process.
Albumen
The compound is synthesized in the liver. If we talk about concentration, then protein accounts for up to 50% of the total amount of substances in plasma.
Albumin performs several important functions:
- Transportation. Transferring connections from place to place. If compared with the liquid fraction itself, the mechanism here will be somewhat different. Albumin binds substances, personally participating in transfer. This is not a purely mechanical action.
Thanks to this ability, it can transport drugs, hormones and all important compounds, chemically active structures.
- Metabolism. Without albumin there can be no normal metabolism. Including energy.
- Regulation of local pressure. We are talking about an indicator in which foreign substances freely pass into the cells. If there is not enough protein, disruptions in the functioning of the entire body begin. Since albumin regulates both metabolism and local pressure at the molecular level. All deviations become noticeable immediately.
- Protein synthesis. Albumin in some cases acts as a building material. When it is processed, other substances are formed. The process is constant and proceeds almost without interruption.
- Preservation of amino acids. Reservation. In this situation, albumin acts as a kind of bank. For the time being, until amino acids are needed.
Albumin is one of the most important proteins in liquid connective tissue. It works both as transport and as a storehouse of important substances. And in some cases it performs tasks related to the synthesis of other chemical molecular structures.
Functions and tasks of plasma
Why does the human body need plasma?
Its functions are varied, but basically they come down to 3 main ones:
- Transporting blood cells and nutrients.
- Establishing communication between all body fluids that are located outside the circulatory system. This function is possible due to the ability of plasma to penetrate the vascular walls.
- Providing hemostasis. This involves controlling the fluid that stops bleeding and removing the resulting blood clot.
Functions of blood plasma
Proteins perform several important functions in the body, one of which is nutritional: blood cells capture proteins and break them down through special enzymes, making the substances better absorbed. The biological substance comes into contact with organ tissues through extravascular fluids, thereby maintaining the normal functioning of all systems - homeostasis. All plasma functions are determined by the action of proteins:
- Transport. The transfer of nutrients to tissues and organs is carried out thanks to this biological fluid. Each type of protein is responsible for transporting a particular component. The transport of fatty acids, medicinal active substances, etc. is also important.
- Stabilization of osmotic blood pressure. The fluid maintains the normal volume of substances in cells and tissues. The appearance of edema is explained by a violation of the composition of proteins, which leads to a failure of the outflow of fluid.
- Protective function. The properties of blood plasma are invaluable: it supports the functioning of the human immune system. The liquid from blood plasma contains elements that can detect and eliminate foreign substances. These components are activated when a focus of inflammation appears and protect tissues from destruction.
- Blood clotting. This is one of the key tasks of plasma: many proteins take part in the process of blood clotting, preventing its significant loss. In addition, the fluid regulates the anticoagulant function of the blood and is responsible for preventing and dissolving blood clots through platelet control. Normal levels of these substances improve tissue regeneration.
- Normalization of acid-base balance. Thanks to plasma, the body maintains a normal pH level.
How to get plasma?
Plasma is obtained from the blood using centrifugation. The method allows you to separate plasma from cellular elements using a special apparatus without damaging them . The blood cells are returned to the donor.
The plasma donation procedure has a number of advantages over simple blood donation:
- The volume of blood loss is less, which means less harm is caused to health.
- Blood can be donated for plasma again after 2 weeks.
There are restrictions on plasma donation. Thus, a donor can donate plasma no more than 12 times per year.
Plasma donation takes no more than 40 minutes.
Plasma is the source of such important material as blood serum. Serum is the same plasma, but without fibrinogen, but with the same set of antibodies. They are the ones who fight pathogens of various diseases. Immunoglobulins contribute to the rapid development of passive immunity.
To obtain blood serum, sterile blood is placed in an incubator for 1 hour. Next, the resulting blood clot is peeled off the walls of the test tube and placed in the refrigerator for 24 hours. The resulting liquid is added to a sterile vessel using a Pasteur pipette.
Technique for obtaining blood, serum and plasma.
Receiving blood. Small amounts of blood from animals are usually taken from the auricle; for this purpose, the collection site is pre-treated, clipped or shaved. Wipe with a swab moistened with 70% alcohol, after which either an incision is made in the vessel or the vein is pierced with a needle. The first drop that appears is removed with a swab, since after treatment with alcohol the red blood cells in it are destroyed. Then the blood is collected drop by drop into a watch glass and immediately pipetted for testing. Blood is taken from the person's middle or ring finger of the left hand, after wiping it with 70% alcohol. A large amount of blood from a horse, cattle, or small cattle is taken from the jugular vein at the border of the upper and middle third of the neck. To do this, a tourniquet is placed on the animal’s neck below the puncture site to fill the vein with blood, wipe it with alcohol or tincture of iodine, then a sterile sharp needle is inserted into the vein at an angle of 45 degrees against the blood flow towards the head. Blood is collected in test tubes or flasks. In pigs, large quantities of blood are obtained from the tail. To do this, cut off about 1 cm of the tail with a scalpel, collect the blood in test tubes, then compress the tip of the tail with an elastic band or bandage for 1-2 days, and thoroughly disinfect the wound. In dogs, large quantities of blood are obtained from the saphen vein (outer thigh). In rabbits from the ear vein, in guinea pigs from the heart, in chickens from the crest or crane vein.
Obtaining blood serum. To obtain blood serum, it must clot; for this, the blood is collected in clean, dry test tubes, a stream of blood is directed along the wall of the test tube to prevent foam from forming, then the test tubes with blood are placed in a thermostat for several hours for complete coagulation, then the resulting clot is separated from the walls of the test tube with a glass rod: circling the clots around, then the blood is settled or centrifuged, while the clot becomes compacted - retraction and a straw-yellow serum is released from it.
Obtaining blood plasma. The blood must be protected from clotting, that is, stabilized. Anticoagulants are used to stabilize the blood. These include Na citrate, Na oxalate, and heparin. An anticoagulant is placed in a test tube, then blood is drawn. After taking, the test tube is carefully inverted several times to mix. When settling or centrifuging, the blood is divided into 2 layers: On top there is a yellowish cloudy liquid-plasma, below there is a dark cherry-colored layer of red blood cells, and on it there is a small white coating of leukocytes.
Blood serum differs from plasma in that it does not contain the protein fibrinogen, since undissolved fibrin is formed from it, which became the basis for a blood clot.
In order to obtain serum from plasma, the fibrinogen protein must be precipitated from it. Then centrifuge and sediment the serum into a separate tube. TCA-trichloroacetic acid.
Determining the volume ratio between plasma and blood cells is the hematocrit indicator.
The blood contains 55-60% plasma of 40-45 formed elements. To determine the hematocrit, stabilized blood (with the addition of an anticoagulant) is used. A little stabilized blood is placed on a watch glass. Take 2 capillary tubes. Both capillaries are filled with blood. Then both ends of the capillary are plugged with plasticine, then placed in a special centrifuge and centrifuged at 3-4 thousand rpm for 8-10 minutes. The capillaries are removed. The blood in them is divided into 2 layers. From the center there is plasma, from the periphery there are formed elements. Then the capillaries are placed in a special frame. The amount of plasma in both capillaries is determined and the average value is taken.
Formed elements of blood.
1. Red blood cells. Red blood cells in higher animals are round, nuclear-free, 5-6 macromeres in diameter, covered on top with a protein-serous membrane, inside the stroma it is represented by hemoglobin. Hemoglobin is a pigment, which in structure is a complex protein consisting of a simple globin protein and a heme coloring substance, which is a prosthetic part. Hemoglobin consists of 4 peroid rings in the center of which is divalent iron. In cross-section, the red blood cell has a biconcave disk to increase its surface area.
2. Leukocytes are white blood cells, larger than red blood cells, contain a nucleus, and are capable of independent movement both in the bloodstream and beyond. Based on their structure and color reproduction, they are divided into 2 groups: granular (granulocytes) and non-granular (agranulocytes). Granular cells include basophils, eosinophils, and neutrophils. Based on the degree of maturity, neutrophils are divided into young, band and segmented.
Agranulocytes-lymphocytes (small, medium, large). Monocytes. In all animals and humans, segmented neutrophils and lymphocytes predominate with different variations.
Hemoglobin is a complex protein that is found inside red blood cells and makes up its stroma. Hemoglobin, due to divalent iron in the composition of heme, can attach oxygen-oxyhemoglobin, this is not a strong compound, it is formed in the vessels of the lungs, releases oxygen into the tissue fluid and is restored. The compound of hemoglobin with carbon dioxide is carbhemoglobin, it is formed in tissues and transported in the lungs. Carbohemoglobin easily releases carbon dioxide and attaches oxygen.
Cito! - Fast. A triad of express blood tests is the hemoglobin level, the number of leukocytes in the blood and the erythrocyte sedimentation rate. In order to determine the level of hemoglobin, it is necessary to destroy red blood cells and release the hemoglobin into solution.
Physiological compounds of hemoglobin are oxyhemoglobin, carbhemoglobin, reduced. There are more than 50 pathological types of hemoglobin. Of these, carboxyhemoglobin is a compound of hemoglobin with carbon monoxide, a very strong compound, methemoglobin is a compound in which iron changes its valence and becomes trivalent and this also leads to the formation of very strong compounds.
ESR (erythrocyte sedimentation rate).
If you take blood stabilized with sodium citrate and draw it into a capillary, place the capillary vertically, the red blood cells will begin to settle, and plasma will remain on top. The erythrocyte sedimentation rate may vary. It depends on several factors, on the type of animal. The highest erythrocyte sedimentation rate in a horse is 64 mm/h. In cattle and small cattle, rabbits 0.5-1 mm/h, in dogs 2.5 mm/h, in pigs 34 mm/h, in humans 4-8 mm/h. In addition, the ESR may change for each individual throughout his life. Under physiological conditions, that is, normally, the ESR does not change significantly, but in a female individual in the 2nd half of pregnancy, the ESR increases significantly. Most often, ESR accelerates or slows down due to pathologies.
For example, ESR slows down when the blood thickens, accelerates when there are inflammatory processes in the body during which many protective globulin proteins are formed, they are adsorbed on red blood cells, lowering their surface charge and red blood cells will settle faster in the blood column. ESR is an important diagnostic indicator and is one of the three express blood tests.
Hemolysis of red blood cells. This is the destruction of the membrane of red blood cells and the release of hemoglobin into solution. There are several types of hemolysis:
1. Osmotic.
2. Chemical.
3. Temperature.
4. Mechanical.
Osmotic hemolysis is based on the fact that in hypotonic solutions red blood cells are destroyed depending on their concentration, and the red blood cells of different individuals are destroyed differently in hypotonic solutions - this means that red blood cells have osmotic resistance - this is the ability of red blood cells to withstand low osmotic pressure.
Chemical is based on the destruction of red blood cells under the influence of chemicals (ammonia, distilled water, acids).
Temperature is based on the destruction of red blood cells after thawing, previously frozen red blood cells. Mechanical when stirring.
Blood clotting.
Blood clotting is a protective reaction of the body that protects it from blood loss. Blood clotting is triggered when the integrity of the vascular wall is violated, due to mechanical or other damage, or when roughness appears on the vascular wall. There are 3 categories of substances in the blood that are involved in blood clotting:
1. Substances that promote coagulation. They combine to form the blood coagulation system.
2. Substances that prevent blood clotting. They combined into an anti-coagulation system.
3. The system of substances that cause the liquefaction of already coagulated blood is the fibrinolytic system.
Blood coagulation consists of the interaction of their components:
1. Hemostasis - stopping blood flow.
2. Reflex narrowing of damaged blood vessels up to spasm.
3. Humoral narrowing under the influence of hormones and mediators adrenaline, serotonin, norepinephrine.
4. Aggregation (sticking) of platelets to each other and their damage.
Blood coagulation system.
There are 13 coagulation factors:
I. Fibrinogen is a blood plasma protein that, when exposed to an unusual environment, turns into an insoluble phase—fibrin.
II. Prothrombin is an inactive form of an enzyme that, under certain conditions, is converted into active thrombin.
III. Thromboplastin is an enzyme released from platelets that activates prothrombin.
IV. Ionized calcium participates in all phases of coagulation and activates all enzymes.
V. Accelerin (Ac) is an enzyme that accelerates the activation of thromboplastin.
VI.
VII. Proconvertin is similar to factor 5 and is involved in the formation of thromboplastin.
VIII. Antihemophilic globulin A. Participate in education
IX. Antihemophilic globulin B. Thromboplastin .
X. Plasma thrombotropin – participates in the formation of a blood clot.
XI. Plasma prothromboplastin.
XII. Hageman factor. It activates prothromboplastin.
XIII. Fibrin stabilizing factor (FSF).
Blood coagulation occurs in 3 phases and is a chain of enzymatic reactions. The result of each enzymatic reaction becomes the trigger for the next enzymatic reaction.
A chain of enzymatic reactions precedes the next reaction. This is a reflex spasm of the injured vessel and the formation of a “platelet nail”. Its formation begins with a change in the charge of the vascular wall at the site of damage. A charge change occurs. This leads to the fact that the formed elements begin to crowd around the damaged area. A special role belongs to platelets. They crowd together and stick together (aggregation), which leads to primary hemostasis. Platelet aggregation leads to their disruption. BAS come out of them, which trigger enzymatic coagulation (coagulation hemostasis). There are three phases in it:
1. When platelets are destroyed, thromboplastin is released from them, which is called blood thromboplastin. Tissue thromboplastin is released from the damaged vascular wall. Normally, they are absent in the body and are released only when the wall is damaged. With their participation, the enzyme blood and tissue prothrombinase is formed. This occurs under the influence of 5 8 9 10 and 11 factors with the participation of calcium ions.
2. Consists in the activation of prothrombin and its conversion into active thrombin under the influence of 5 7 factors and in the presence of calcium ions.
3. Consists in the formation of fibrin. Goes in 3 stages:
a. Proteolytic stage. Thrombin acts on fibrinogen, splits off individual monomers from it, and profibrin is formed.
b. Polymerization. With the participation of calcium, profibrin molecules stick together. Fibrin polymer is formed.
c. Under the influence of factor 8, fibrin polymer molecules are cemented. The final fibrin is formed. It falls out in the form of threads, the formed elements become entangled in them, and a clot is formed.
This is not the final stage, since after some time the fibrin filaments begin to shorten, which causes the clot to thicken and the liquid-serum to be squeezed out of it. Compaction of a clot by retraction is a complex biological process that leads to a tight closure of the vessel with a plug, thus bringing the edges of the wound closer together. The fibrin plug dissolves over time. This fibrinolysis process is carried out under the action of the fibrinolytic system.
Blood pathologies affecting the nature of plasma
In medicine, there are several diseases that can affect the composition of plasma. All of them pose a threat to human health and life.
The main ones are:
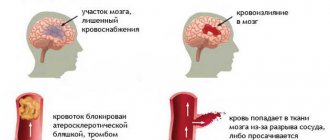
- Hemophilia. This is a hereditary pathology when there is a lack of protein, which is responsible for coagulation.
- Blood poisoning or sepsis. A phenomenon that occurs due to infection entering directly into the bloodstream.
- DIC syndrome. A pathological condition caused by shock, sepsis, severe injuries. It is characterized by blood clotting disorders, which simultaneously lead to bleeding and the formation of blood clots in small vessels.
- Deep venous thrombosis. With the disease, the formation of blood clots in the deep veins (mainly in the lower extremities) is observed.
- Hypercoagulation. Patients are diagnosed with excessive blood clotting. The viscosity of the latter increases.
Plasma test or Wasserman reaction is a study that detects the presence of antibodies in plasma to Treponema pallidum. Based on this reaction, syphilis is calculated, as well as the effectiveness of its treatment.
Plasma, a liquid with a complex composition, plays an important role in human life. It is responsible for immunity, blood clotting, homeostasis.
What is the difference between blood and plasma?
What is the difference between blood and blood plasma? Their difference is as follows. Plasma is a component of blood, in addition to which there are also formed cells: red blood cells, platelets, leukocytes and others.
Plasma itself consists of water and components dissolved in it: proteins, inorganic substances, minerals. Relative difference in chemical composition.
They differ in color. Blood is red because it contains hemoglobin, which is made up of red blood cells. Plasma is yellow in color and transparent.
Important!!! The color of the plasma reflects the state of the body. For example: a green tint will appear due to a dysfunction of the immune system, gray - due to a malfunction of the pancreas.
Globulins
The remaining plasma proteins are classified as globulins, which are large in molecular weight. They are produced in the liver and in the organs of the immune system. Main types:
- alpha globulins,
- beta globulins,
- gamma globulins.
Alpha globulins bind bilirubin and thyroxine, activate the production of proteins, transport hormones, lipids, vitamins, and microelements.
Beta globulins bind cholesterol, iron, vitamins, transport steroid hormones, phospholipids, sterols, zinc and iron cations.
Gamma globulins bind histamine and participate in immunological reactions, which is why they are called antibodies, or immunoglobulins. There are five classes of immunoglobulins: IgG, IgM, IgA, IgD, IgE. Produced in the spleen, liver, lymph nodes, and bone marrow. They differ from each other in biological properties and structure. They have different abilities to bind antigens, activate immune proteins, have different avidity (rate of binding to antigen and strength) and ability to pass through the placenta. Approximately 80% of all immunoglobulins are IgG, which have high avidity and are the only ones that can cross the placenta. IgM is synthesized first in the fetus. They are also the first to appear in the blood serum after most vaccinations. They have high avidity.
Blood composition
Fibrinogen is a soluble protein that is produced in the liver. Under the influence of thrombin, it is converted into insoluble fibrin, due to which a blood clot is formed at the site of vessel damage.
Plasma composition and functions of its elements
Most of the plasma is water, its amount is approximately 92% of the total volume. In addition to water, it includes the following substances:
- proteins;
- glucose;
- amino acids;
- fat and fat-like substances;
- hormones;
- enzymes;
- minerals (chlorine, sodium ions).
About 8% of the volume is proteins, which are the main part of plasma. It contains several types of proteins, the main ones being:
- albumins – 4-5%;
- globulins – about 3%;
- fibrinogen (belongs to globulins) – about 0.4%.
Application in donation
In what situations and why is donor blood plasma needed? Most often, plasma is not transfused with whole blood, but only with its components and plasma liquid. When collecting blood, the liquid and formed elements are separated using special means, the latter, as a rule, are returned to the patient. With this type of donation, the frequency of donation increases to twice a month, but no more than 12 times a year.
Donor plasma transfusion
Blood serum is also made from blood plasma: fibrinogen is removed from the composition. At the same time, the serum from the plasma remains saturated with all the antibodies that will resist microbes.