Hypoplastic anemia
(Greek hypo- + plasis formation, formation; anemia; synonym:
aplastic anemia, aregenerative anemia, hemorrhagic aleukia, myelophthisis, myelophthisis, panmyelophthisis, progressive hypocythemia
) - a disease of the blood system, characterized by inhibition of the hematopoietic function of the bone marrow and manifested by insufficient formation of red blood cells , leukocytes and platelets (panhemocytopenia) or red blood cells alone (partial hypoplastic anemia, erythroblastophthisis).
Hematopoiesis
Before characterizing a disorder of the hematopoietic system, it is worth understanding how cells mature.
The bone marrow is the only hematopoietic organ in the body. It is located in spongy bones and epiphyses of tubular bones. Proliferation (increase) in the number of cells occurs through mitosis, that is, cell division with an even distribution of genetic material.
Cell maturation occurs between divisions. Various substances help them in this: hematopoietic growth factors, interferons, lymphokines, chemokines and others. They additionally activate and regulate immune responses. Several hematopoietic sprouts are distinguished.
There are several stages for a stem cell to develop into a mature blood cell. As can be seen from Scheme 1, a cell gives rise to others, which in turn are the predecessors of others, and so on. Blast cells make it possible to morphologically recognize which path the differentiation process takes. As cells reach functional maturity, they lose their ability to divide.
The final stage of hematopoiesis is the release of mature functionally active cells into the bloodstream.
General concepts about hypoplastic anemia
Hypoplastic anemia is a pathological change in the blood picture due to suppression of the red bone marrow. This is manifested by a decrease in the production of all blood germs (erythrocyte, leukocyte, platelet) or only red (decreased red blood cells). The history of the first description and appearance of this disease begins in 1888. At this time, P. Ehrlich identified a disease in the girl, manifested by the acute development of bleeding, fever, deep anemia and leukopenia. According to the results of the autopsy and bone marrow examination, no signs of hematopoietic disorders were identified. Anaplastic anemia as an independent disease was identified by Shoffar in 1904. Later, aplastic anemia of the Ehrlich type appeared with symptoms of sepsis, necrosis, hemorrhage and aplasia (the absence of all hematopoietic germs in the bone marrow), which manifests itself in young people (18–20 years old). The main population suffering from this disease are young girls and children. There are several stages in the pathogenesis of development. First, tissues, due to lack of oxygen and nutrients, atrophy and lose their functions. Next, adipose and connective tissue replace the dead cells, which leads to the spread of the pathological process. The progression of the disease occurs very quickly and, if left untreated, can lead to death.
Prevalence of aplastic anemia
On average, 2–3 cases per year occur per 1 million population. There is a dependence on the area - the figure is 2 times higher in the Far East. Race doesn't matter. There are 2 peaks of occurrence: in young people (14 – 25 years old) and elderly people (60 years old). It occurs equally in men and women.
Hypoplastic anemia in children
Signs of progression of hypoplastic anemia in children appear quite late, most often this occurs between the ages of 4 and 12 years. However, their manifestation is a little more noticeable than in adults - this is due to the accelerated development of the child’s body. Children with this form of anemia have multiple malformations of the heart muscle, kidneys, and skeletal system. Older children complain of pain in the heart area and feel “freezing.”
Causes
When the reasons that caused the development of the disease are unknown, it is called idiopathic. This happens in most cases. But sometimes it is still possible to establish the cause. She may be:
- the effect of ionizing radiation;
- toxins – benzene, insecticides;
- medications – chloramphenicol, non-steroidal anti-inflammatory drugs, cytostatics;
- hepatitis, Ebstein-Barr viruses;
- diseases of the immune system;
- genetic disorders during the maturation of bone marrow cells.
Some sources indicate that aplastic anemia may develop during pregnancy.
Classification
Depending on the origin, hypoplastic anemia is:
- congenital. Symptoms of the disease appear in early childhood and progress rapidly. The causes of development may be genetic mutations of DNA in the fetus; hereditary predisposition (there is evidence of a similar anomaly in one of the relatives); impaired intrauterine development (pathological changes in the fetal hematopoietic system under the influence of an unfavorable factor). Studies have shown that boys suffer from congenital aplastic syndrome twice as often as girls;
- acquired. This type of hypoplastic anemia is typical for any age group.
There are idiopathic (the cause of the disease is unknown) and myelotoxic (the prerequisite is the toxic effect of an external factor) forms. The reasons that determine the development of myelotoxic form of anemia include:
- chronic intoxication with chemicals;
- medications with side effects on hematopoiesis (hormonal, tranquilizers, cytostatics);
- exposure of the body to high doses of radiation (radiologists are susceptible);
- diseases of the endocrine system (may be complicated by hypoplastic anemia);
- effects of viruses on blood cells;
- against the background of tuberculosis and pregnancy, hypoplastic anemia can also develop, but such cases are rare in medical practice.
Depending on the duration of the disease, there are:
- Acute anemia (lasts up to 4 weeks).
- Subacute (lasts 1–6 months).
- Chronic (present for more than six months).
Depending on the severity of damage to bone marrow functions, there are pathologies:
- Moderate severity. The disruption of hematopoietic elements occurs selectively, while maintaining minimal formation of full-fledged blood cells.
- Severe severity. The bulk of the bone marrow atrophies and is replaced by adipose tissue. 30 percent of the bone marrow is functionally active.
- Extremely severe. There is an almost complete loss of function by the bone marrow and its replacement with adipose tissue.
Depending on the affected blood sprouts, the following are distinguished:
- Erythrocytopenia, or partial hypoplastic anemia (suppression of erythrocyte hematopoiesis).
- Erythrocyte-, thrombocytopenia (decreased production of red blood cells and platelets).
- Pancytopenia, or true hypoplastic anemia, (reduced production of all blood cells).
According to the International Classification of Diseases (ICD-10), anaplastic anemia has code D60 (erythroblastopenia - acquired red cell aplasia), D61 (other aplastic anemia).
Mechanism of development of the pathological process
The presence of a defect in stem cells or a decrease in the number leads to their low proliferative activity. Another mechanism for the development of aplastic anemia is a violation of the regulation by immunocompetent cells of the processes of maturation of blood sprouts (hematopoiesis). Pathology of the microenvironment is one of the possible ways leading to inhibition of blood cell synthesis or their complete absence.
A combination of several mechanisms in the development of aplastic anemia is possible.
Treatment
Treatment of aplastic anemia, despite the seemingly identical symptoms, is prescribed by doctors depending on the presumed main factor in the etiology of the disease.
Newly identified cases are necessarily treated in the hematology department as an inpatient. Only specialized therapy allows you to choose the right dosage and the optimal drug.
Basic techniques:
- transfusion of donor blood or individual elements for replacement purposes;
- bone marrow transplantation;
- medications that activate hematopoiesis.
For transfusion, whole blood, erythrocyte and platelet mass, and granulocytes are used. They are prepared at “Transfusion Stations” from the blood of donors. The method is considered temporary because it simply replenishes the missing number of one’s own blood cells, but does not affect the bone marrow. If the autoimmune mechanism of the pathology is proven, it cannot be used. The body produces antibodies to foreign cells.
Frequent transfusions lead to the accumulation of iron and its deposition in internal organs, disrupting their functioning. This forces the addition of drugs that help remove iron from the blood.
Bone marrow collection for transplantation is carried out in an operating room by puncturing the femur, and up to 2 liters of the mass is sucked out with syringes.
Bone marrow transplantation is the most effective treatment option. Blood transfusions are stopped before the procedure to reduce the possibility of rejection. A relative with the same blood type and individual compatibility can become a donor. The method is more indicated when the patient is young.
Before transplantation, radiation and chemotherapy are performed. It is necessary to suppress a possible immune response to rejection of the donor's stem cells. The method is carried out only in specialized departments and is expensive.
The following are used as immunosuppressants: Cyclosporine, antimonocyte and antilymphocyte globulins. A complex drug of this group is Atgam (contains the necessary antiglobulins). It is indicated in cases where bone marrow transplantation is not possible. Corticosteroids are used to prevent anaphylactic reactions.
Stimulation of hematopoiesis in the bone marrow is carried out using drugs such as Filgrastim, Leukomax. They activate the production of granulocytes, therefore they are indicated only for leukopenia. The course of treatment is two weeks.
The ability of male sex hormones (androgens) to stimulate all blood growths has been proven. For the treatment of men, long courses of Testosterone propionate and Sustanon are used.
Removal of the spleen is effective in 85% of patients. The method is based on the mechanism of stopping the production of antibodies to one’s own cells. Can be performed on all patients who do not have infectious complications.
Medicines are administered primarily by injection
If the patient has bleeding, hemostatic agents are administered: Dicinone, Aminocaproic acid.
The removal of iron from the body is achieved with the help of Desferal.
Treatment of aplastic anemia with folk remedies should be abandoned. This pathology requires very thoughtful and accurate accounting of medications. How can you calculate the beneficial components in plants? There are references to the stimulating effect of garlic, red clover, radish, carrots and beets. But it is so small that its use only raises unreasonable hopes among patients and relatives.
Clinical manifestations of aplastic anemia
All the main symptoms of aplastic anemia occur due to a deficiency of blood cells and impaired function. A deficiency of platelets leads to the development of hemorrhagic syndrome, leukocytes (agranulocytosis) - reduced immunity, erythrocytes - anemic syndrome.
As noted earlier, acute and chronic course of aplastic anemia is possible. In 15% of patients, the disease is acute and is accompanied by elevated body temperature and multiple hemorrhages. In the congenital form (Fanconi anemia), growth and development delays and “coffee” spots on the skin are possible.
Anemic syndrome is manifested by dizziness, flashing “spots” before the eyes, and weakness.
Leukocytopenia - a low level of white blood cells is accompanied by the addition of a bacterial infection.
Hemorrhagic syndrome - manifested by bleeding (nose, gum, uterine), rashes on the skin. With hemorrhage in the fundus of the eye, this may manifest itself as a decrease in visual acuity. Most often this is typical for young people with severe aplastic anemia.
Symptoms
All symptoms of aplastic anemia are combined into 3 main groups of syndromes: anemic syndrome, hemorrhagic syndrome, syndrome of infectious complications.
Anemic syndrome is characterized by:
- severe general weakness;
- rapid fatigue;
- intolerance to habitual physical activity;
- shortness of breath and tachycardia with moderate exertion, in severe cases - at rest, when changing body position;
- headaches, dizziness, episodes of fainting;
- noise, ringing in the ears;
- feeling of a “stale head”;
- flickering of “flies”, spots, colored stripes before the eyes;
- stabbing pain in the heart area;
- decreased concentration;
- Violation of the sleep-wake pattern (drowsiness during the day, insomnia at night).
Objectively, when examining patients, pallor of the skin and visible mucous membranes, muffled heart sounds, increased heart rate, and decreased blood pressure are established.
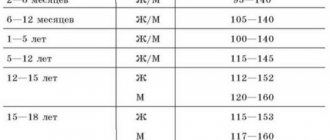
There are two peaks of incidence: at 10–25 years and after 60 years. Women get sick more often.
Hemorrhagic syndrome manifests itself:
- hematomas (bruises) of various sizes and pinpoint hemorrhages that occur on the skin and mucous membranes after minor exposure or spontaneously, for no reason;
- bleeding gums;
- bleeding from the nose;
- in women - uterine intermenstrual bleeding, prolonged heavy menstruation;
- pink staining of urine;
- determination of traces of blood in feces;
- possible massive gastrointestinal bleeding;
- hemorrhages in the sclera and fundus;
- hemorrhages in the brain and its membranes;
- pulmonary hemorrhages.
Objective confirmation of hemorrhagic syndrome is pinpoint hemorrhages and bruises on the skin and mucous membranes, multiple hematomas at different stages (from purple-violet to yellow).
Infectious complications are represented by developing pneumonia, pyelonephritis, furunculosis, post-injection abscesses or infiltrates, and in severe cases - sepsis.
Signs of aplastic anemia in children
In childhood, congenital pathology is more often observed, transmitted from parents or acquired during intrauterine development. Some signs of this pathology can be detected even in a newborn, others may appear only after a few years. Severe symptoms of anemia in newborns include:
- anomalies of the facial structure (triangular face, small eyes, snub nose, etc.);
- limb anomalies (absence of a thumb, absence of the radius, six-fingered fingers, etc.);
- short stature;
- features of skin pigmentation are clusters of multiple spots of light brown color;
- anomalies of internal organs, most often the genitourinary system;
- deformation and destruction of nails;
- mental retardation;
Aplastic anemia in children over 1 year of age is initially determined by appearance and behavior. Sick children differ from their peers in the pallor of their skin and mucous membranes, they experience an increase in the size of the lymph nodes, frequent bleeding from the nose and gums, and blood in the urine in the morning. Their behavior is characterized by frequent mood swings, irritability, they quickly get tired and lose their appetite.
Diagnostics
The diagnosis is confirmed on the basis of clinical symptoms, laboratory and instrumental research methods. The characteristic symptoms of aplastic anemia are listed above.
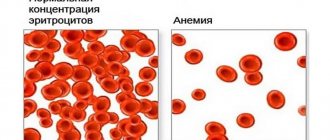
The first laboratory test is a general blood test, which reflects the level of all formed elements. As has been mentioned more than once, there will be pancytopenia - low levels of blood cells.
Detected anemia is characterized by a color indicator. In aplastic anemia, it is normochromic or may have slight hyperchromicity. Reticulocytes are reduced or absent. ESR (erythrocyte sedimentation rate) readings will be increased. A low level of leukocytes occurs due to a deficiency of granulocytes, and relative lymphocytosis is noted. The structure of platelets and their functional abilities are disrupted.
A bone marrow puncture is performed. The characteristics of the resulting punctate will depend on whether the needle entered the depressed lesion or the remnants of normally functioning bone marrow. In the first case, the punctate will be depleted of cellular elements, the number of young forms of granulocytes will be reduced, the percentage of lymphocytes will be increased, and the processes of differentiation and proliferation will also be disrupted.
The detection of blast cells in punctate is not related to aplastic anemia, which means that one should look for another pathological process similar to this in clinical manifestations and disorders of the maturation of hematopoietic cells.
There is deposition of excess iron in the form of pigment in the liver, spleen, and bone marrow. For a correct diagnosis, it is necessary to find out what could lead to a reduced level of leukocytes (toxic substances, medications, infectious agents, autoimmune lesions, chronic inflammatory processes, hypothyroidism).
Anemia similar to aplastic anemia can occur with partial red cell aplasia. In this condition, the processes of synthesis and differentiation of erythroid cells are disrupted in isolation, and the production of antibodies to bone marrow cells is possible.
The diagnosis of aplastic anemia is made if any 2 of the following criteria are present:
- hemoglobin level less than 100 g/l;
- leukocyte level less than 3.5 * 109 / l (granulocyte content less than 1.5 * 109 / l);
- hypocellular bone marrow and platelet level less than 50 * 109/L.
Characteristics of the severity of aplastic anemia are presented in Table 1.
Table 1. Criteria for the severity of aplastic anemia.
| Severity | Criteria |
| Moderate |
|
| Heavy |
|
| Very heavy |
|
Determining the severity of aplastic anemia is important when prescribing therapy and the timing of its implementation.
Symptoms and diagnosis
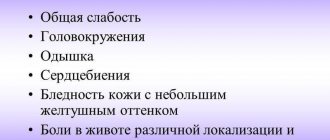
Signs of hypoplastic anemia are:
- General weakness.
- Malaise.
- Dizziness. The cause of this symptom is oxygen deficiency in the brain due to a decrease in the number of red blood cells.
- Fast fatiguability.
- Decreased performance.
- Pale color of the skin and mucous membranes.
- Noise in ears.
- Shortness of breath that occurs during physical exertion.
- Tingling in the chest.
- Fainting.
- Floaters before the eyes.
- Daytime sleepiness.
- Sleep disturbance.
- Chest pain.
- Bleeding and hemorrhage.
- Petechial rash.
- Bleeding gums.
- Signs of damage to the oral mucosa.
- Menorrhagia (heavy periods).
- Nosebleeds.
Congenital hypoplastic anemia can be combined with microcephaly (reduction in brain size), slow growth of the child, impaired skin pigmentation, hearing loss and congenital abnormalities of various organs.
The diagnosis is made by a hematologist based on anamnesis; for diagnosis, the following is carried out:
- Physical examination. Valuable diagnostic signs of this form of anemia are the absence of lymphadenopathy and the normal size of the spleen and liver.
- Examination of the skin and mucous membranes. Often with this pathology, ulcerative-necrotic changes in the mucosa are detected.
- General blood analysis. Detects a decrease in leukocytes, erythrocytes and platelets, or only erythrocytes. With a low hemoglobin level, the color indicator is within normal limits. The number of neutrophils decreases.
- General urine analysis. In the urine of patients, red blood cells are often found (the cause is hemorrhagic syndrome), bacteria (in case of infection) and a large number of leukocytes.
- Blood chemistry.
- Puncture followed by examination of punctate. There is a decrease in the number of megakaryocytes and myelokaryocytes.
- Trephine biopsy. Detects a decrease in the volume of functional tissue.
- Electrocardiography.
- Other instrumental studies (FEGDS, sigmoidoscopy, colonoscopy, salpingography) are performed for bleeding.
Important information: How to treat chronic anemia
Differential diagnosis is carried out with other anemias (iron deficiency, posthemorrhagic, thalassemia, hemolytic) and blood cancer.
Treatment of aplastic anemia
The main treatment method for aplastic anemia is to restore the number of hematopoietic cells, as well as prescribe immunosuppressive therapy to suppress immune reactions. The most effective method is hematopoietic stem cell transplantation.
During bone marrow transplantation, donor and recipient compatibility must be carefully assessed to avoid graft-versus-host disease.
It is noted that for aplastic anemia caused by chemotherapy and congenital forms, immunosuppressive therapy is not effective.
Immunosuppressive therapy includes:
- antilymphocyte immunoglobulin;
- cyclosporine;
- glucocorticoids;
- cytostatics.
Please note that you should not self-medicate, since each medicine has its own indications, contraindications, and side effects.
It is not allowed to use immunosuppressive drugs in the presence of an infectious-inflammatory process, severe disorders of the cardiovascular system, liver, kidneys, or intractable hemorrhagic syndrome.
With any therapy, patient monitoring by medical personnel is necessary to assess possible allergic reactions that may occur to the components of the drug. There may be a delayed allergic reaction that appears after 2 to 3 days.
The use of growth factors ensures the maintenance of granulocytes at a level of 1 – 1.5 * 109/l. Lymphocytoplasmapheresis may be prescribed as an additional treatment method. It is justified in the presence of an allergic reaction or the formation of antibodies to blood cells. Another direction of treatment for aplastic anemia is therapy against the main complications: infectious, hemorrhagic, allergic. In some cases, platelet and red blood cell transfusions are performed.
Table 2. Indications for prescribing transfusion of red blood cells and platelet concentrate.
| Blood components for blood transfusion | Indications |
| Red blood cell mass | Hemoglobin less than 90 g/l Hematocrit less than 30% |
| Platelet mass | Bleeding due to low platelet levels (10 – 20 * 109/l) |
Course of the disease
The clinical course of aplastic anemia differs according to the form of the disease.
Acute anemia
The acute form of the disease proceeds rapidly, beginning abruptly with severe hemorrhagic syndrome (bleeding of various types). Infection with high fever (sore throat, pneumonia) occurs. After a few days, an extreme degree of devastation of the bone marrow occurs, inhibition of the erythrocyte germ. Relative lymphocytosis and a significant acceleration of ESR are detected in the blood. Death occurs within 1–1.5 months.
Subacute form
It proceeds less quickly. Hemorrhages are not too pronounced. Critical changes in the blood occur after 3 months or a year.
Chronic form
The disease begins gradually and progresses slowly. The person experiences dizziness, pallor, and intermittent bruising. On examination, no enlargement of the spleen is detected. Palpation of painful lymph nodes is possible. With proper treatment, it is possible to stop the process of bone marrow death. Remissions last up to several years. Exacerbation is provoked by any infection or stress.
Remission - laboratory criteria
To evaluate therapy, the concept of remission is used. Improvement of bone marrow hematopoiesis - incomplete (partial) remission, allows the patient to avoid dependence on blood transfusions. The number of granulocytes in the blood is more than 0.5 * 109/l, which reduces the risk of severe infectious complications. Complete remission is accompanied by the absence of clinical manifestations, the hemoglobin level returns to normal, the platelet count is more than 100 * 109/l, granulocytic leukocytes - 1 * 109/l.
What it is?
The bone marrow of a healthy person is the place where all blood cells - red blood cells, white blood cells and platelets - appear and mature. All these cells are indispensable for the body.
- Red blood cells carry oxygen and carbon dioxide, and when they are deficient, the brain is the first to suffer from oxygen starvation. A lack of red blood cells is called anemia.
- White blood cells are responsible for fighting viral, bacterial and fungal infections. If there are not enough of them, the person is haunted by constant, severe inflammatory diseases.
- Platelets are responsible for blood clotting. When their number is below a critical level, causeless bleeding and hemorrhage appear - hemorrhagic syndrome (“hemos” - blood, “rragia” - flow).
In aplastic anemia, all these cells are not enough. Hence the manifestations of the disease - anemic, infectious and hemorrhagic syndromes. A similar picture is observed in some cancers, for example, acute leukemia. Therefore, an experienced hematologist must understand the problem.
Prevention
Prevention of the development of aplastic anemia involves limiting the influence of unfavorable external factors on the body. It is necessary to follow safety rules when working with ionizing radiation, benzene, avoid uncontrolled use of medications, treat diseases of organs and systems that lead to a decrease in hematopoiesis, for example, kidney pathology, cirrhosis of the liver.
With confirmed aplastic anemia, it is necessary to monitor the patient's condition, constant monitoring of the levels of formed elements, so as not to miss a relapse and possible complications.
Causes
The hypoplastic anemia in question is caused by impaired hematopoietic functions and bone marrow depletion.
There are several main reasons why this type of anemia can occur in people of different ages:
- Hereditary factor. Experts say the most common cause is hereditary predisposition. One or both parents with anemia and bone marrow problems may pass on a special type of antibody. These antibodies act in a way that prevents the creation of new blood cells.
- Impacts that depress brain function. This includes various reasons that can negatively affect this human organ. This mainly concerns chemotherapy, radiation exposure, the influence of arsenic, benzene and derivatives of this substance.
- Some diseases. A pathology such as tuberculosis can provoke hematopoietic disorders and bone marrow depletion.
- Pregnancy. It is not so common, but due to increased stress on the body, a weakened immune system and deterioration of the general condition, hypoplastic anemia sometimes develops.
- Impact of drugs. They are also considered rare factors influencing the development of hypoplastic anemia. The disease can be provoked by taking potent hematotoxic drugs, antibiotics or cytostatics. Therefore, you should be careful when using any drug and choose them only as prescribed by your doctor.
Here, hypoplastic and aplastic anemia are similar. But the aplastic form of anemia is caused by exposure to large doses of ionizing radiation, benzene, lead compounds, mercury and other severe intoxications. But there is also a functional deficiency in the functioning of the bone marrow, which is explained by a violation of hematopoietic processes.