What it is
An open or closed rupture of a vessel is a violation of its integrity. Accompanied by internal and external hemorrhage.
Lesions of the lower extremities occur more often. In 2nd and 3rd place are the arms and neck. They can occur in combination with lesions of the kidneys, chest, torso, and abdominal cavity.
A rupture of a large blood wall poses a threat to life, when patients are indicated for emergency care in a clinic to stop the hemorrhage.
A blood vessel burst in the head: symptoms, consequences
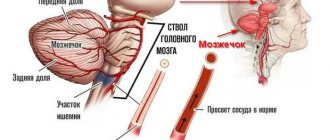
The patient is in serious condition if a vessel in the head bursts. This disorder is called hemorrhagic stroke. As soon as the vessel bursts, blood enters the brain, which leads to various consequences, including death.
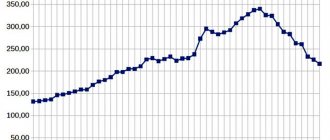
Previously, only elderly people encountered this pathology. Now the disease is getting younger, increasingly affecting people under 40 years of age. 80% of patients who have suffered a stroke are no longer able to return to their previous lives and cope without outside help.
Provoking factors
If there are any disorders in the body, the following factors can provoke a rupture of the vessel:
- Obesity.
- Smoking.
- Depressive state.
- Incorrect diet, fasting.
- Vascular disorders.
- Constant stress, emotional instability.
- Overwork, both physical and mental.
- Large quantities of alcohol.
- Hypertensive crises.
- Acute intoxication with drugs or chemicals.
- Sunstroke, overheating.
- Traumatic brain injury.
Most often, a sick person does not even suspect that he has a damaged vessel in his head. But, for example, if a serious traumatic brain injury occurs, the walls of such a vessel burst and hemorrhage occurs.
How to recognize a stroke and its main symptoms
If a blood vessel bursts in the head, the victim’s symptoms manifest themselves as follows:
- The person is unconscious or in a stupor.
- Convulsions and tremors of the limbs are observed.
- Breathing is either slow or noisy and rapid.
- The eyeballs move randomly or, conversely, the pupils are fixed in the direction of the damaged area.
- The face is curved in one direction (drooping of the corner of the mouth and eyelid is noticeable).
- The occipital muscles are contracted so that the patient is unable to touch the chest with his chin.
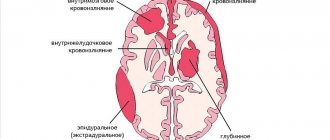
The general condition of a patient experiencing a hemorrhagic stroke is assessed by doctors as severe or critical. It is important to provide timely medical assistance here. Depending on the damaged vessel, up to 150 ml of blood can be thrown into the brain. Its intense current is harmful to neurons. It fills the brain cavities, displaces tissue, leading to edema and necrosis.
How can I help you
You can determine that a person has a hemorrhagic stroke and a burst blood vessel in the brain by inappropriate behavior and a sharp change in his well-being.
Necessary:
- Ask him to smile. With a stroke, the smile will be one-sided, since one half of the body does not work.
- Ask to say your first and last name. The patient's speech will be slurred, slow, and hesitant.
- Suggest raising both hands up. A person either will not be able to do this, or the arm on the damaged part of the body will be lower than the other.
- Ask to stick out your tongue as far as possible. During a stroke, the tongue becomes bent or retracts to one side.
The further fate of the patient is in the hands of the people around him at the time of the attack. The first thing you need to do is call an ambulance. And then, while waiting for the doctors:
- Lay the victim so that the head and shoulders rise above the body. It is important not to allow him to stand up or move around.
- Loosen the straps, unbutton the cuffs and collar of the shirt.
- If you have dentures, you need to get them.
- Turn the patient's head to the side.
- If vomiting, ensure that the mouth is cleaned with a handkerchief or piece of cloth.
- Apply a cold compress to your forehead.
- Rub your palms and feet to improve blood circulation.
You cannot give any medications to the patient yourself. Any erroneous and illiterate action can be fatal.
Consequences of a stroke
When a patient has a blood vessel burst in his head, the consequences can be very disappointing. It all depends on the degree of vascular damage, the location of the hemorrhage and the timeliness of medical care. Often, a stroke ends in death within the first weeks due to the death of neurons and the resulting chemical processes.
If displacement of brain tissue and hemorrhage into the ventricles has not occurred, then the prognosis is more favorable. But even then the person is threatened with:
- Constant attacks of pain in the head.
- Paralysis of the limbs of one half of the body.
- Mental disorders, nervousness.
- Impaired speech, hearing, vision.
- Facial asymmetry.
- Inability to move without support.
- Impaired coordination of movements.
- Deterioration of memory and thought process.
- Lack of consciousness with the functioning functions of breathing and heartbeat.
Consequences and treatment of aneurysm
An aneurysm does not make itself felt for a long time, being a common cause of stroke. A person can live his life calmly, without suspecting that he is in danger. If a cerebral vessel bursts, the consequences of such a rupture due to an aneurysm are as terrible as with a stroke.
What may happen:
- Stroke.
- Vasospasm.
- Coma.
- Hydrocephalus.
With hemorrhage, intracranial pressure sharply increases, the cerebrospinal fluid channels become clogged and the brain structures are displaced. This means that the functions of the affected areas of the body will be lost and may not be restored.
To prevent hemorrhage, surgery is indicated. This procedure is traumatic and poses a huge risk for the patient. It is performed if the size of the aneurysm is more than 10 mm.
The neurosurgical operation involves applying a special clip to the affected vessel. In this case, specialists use a microscope and microsurgical equipment. During endovascular intervention, under CT control, a coil is installed through the femoral artery to exclude the diseased vessel from the bloodstream.
To avoid a blood vessel bursting in your head, you need to pay enough attention to your health. Lead a healthy lifestyle, eat right, give up bad habits and at the first unpleasant symptoms (head pain, dizziness, ringing in the ear) consult a doctor. Timely treatment will help avoid serious consequences.
02.01.2018
(4 4,50 of 5) Loading...
Source: https://BolitGolova.info/mozg/lopnul-sosud-v-golove.html
Causes
Damage to blood vessels is caused by the following reasons:
- fracture;
- falling from height;
- strong blow, bruise;
- stabbing, laceration, gunshot wound;
- connective tissue diseases;
- aneurysms;
- capillary fragility due to inflammation or age-related atherosclerotic changes;
- oncology with tumor growth;
- degenerative processes of the cardiovascular system.
Causes of aneurysm rupture
Vascular and hemodynamic factors predispose to rupture:
- Local thinning of the vessel wall;
- High blood flow speed;
- Fragility of the apex of the aneurysm, which accounts for 95% of complications;
- Chronic concomitant diseases.
The combination of these factors leads to increased load on the affected area of the artery.
Having reached the limit of extensibility, the vascular wall ruptures. The mechanism of damage resembles a burst balloon, from one end of which pumped air (blood) begins to escape. Other risk factors:
- Diabetic angiopathy;
- Hypertonic disease;
- Atherosclerosis;
- Pregnancy;
- Obliterating endarteritis;
- Takayasu's disease;
- Falls and injuries.
What types are at high risk of hemorrhage?
The arterial bed is most often affected, where high blood pressure is observed. The larger the diameter of the artery, the higher the risk.
The predominant localization of atherosclerotic plaques is also important, determining the high frequency of damage to the following arteries:
- Mozgovykh;
- Renal;
- Carotid (read about damage to the carotid artery here);
- Splenic (you will learn what a splenic artery aneurysm is here);
- Abdominal aorta - more than 90% of cases.
Kinds
According to the classifier and the degree of visibility of the wound surface, vascular damage by type is open and closed. The character is a simple rupture, with crushing.
Taking into account the area of localization of the affected venous trunks: on the arms, legs, neck.
Open
With open wounds the following is observed:
- violation of the integrity of the skin;
- partial or complete rupture of the choroid;
- obvious external bleeding from the wound;
- tear or dissection of a blood tube.
Liquor accumulates in the destroyed wall, causing thrombosis, blockage, and compression of surrounding areas. If the liquid does not pour out, it gets compacted in the soft parts, forming a hematoma.
Closed
This is a type of violation of integrity due to a fall, bruise or blow with a blunt object, when the skin remains intact. A banal bruise is a possible rupture of a vessel.
The effusion progresses under the skin, a pulsating hematoma is localized, and the pressure decreases. In case of hemodynamic disturbances and intense bleeding, hemorrhagic shock begins to develop - an acute emergency condition.
There are also occlusive and contusive disorders. The first are caused by a bruise due to a fracture or dislocation of a bone. The second (compression) are ruptures of the middle and inner lining of the arteries.
During contusion, individual or circular cracks appear in the intima. In case of injury to the inner and middle shell, its detachment is observed.
The cerebrospinal fluid is discharged directly into the vein, and the vascular lumen is clogged. A pulsating bruise occurs at the affected area with the formation of a traumatic aneurysm.
If a simultaneous rupture of the venous wall occurs, an arteriovenous fistula breaks out. General circulatory disorders or certain distal areas of the body occur.
Types of vascular injuries
Internal bleeding, damaged internal organs
Depending on whether there are external signs of vascular injury, they are divided into open and closed. The former may be accompanied by a bruise, tear or complete dissection of the vascular wall.
Closed injuries are not accompanied by external bleeding, but they lead to thrombosis, intense internal hemorrhage, tissue ischemia, and aneurysm of the wall of a vein or artery.
The danger to life increases if the main vessel is damaged; it is lower if secondary blood pathways are injured. Depending on the type of injured vessel, there are arterial, venous, capillary and mixed pathologies. Blood flow pathways in the arms, legs and neck, head and torso may be affected. Internal bleeding occurs when the organs of the chest or abdominal cavity are damaged . In the case of polytrauma, all these types are combined with each other.
Based on the nature of vessel ruptures, the following are distinguished:
- full,
- partial,
- through,
- tangentially,
- fenestrating (for puncture, wound by shrapnel).
We recommend reading an article about how post-traumatic thrombosis manifests itself and is treated. From it you will learn about the causes of post-traumatic thrombosis, the clinical picture of the development of the acute form, methods of diagnosis and treatment of the veins of the lower extremities, as well as recovery after treatment and the prevention of thrombosis after injury.
And here is more information about the prevention of blood clots and thrombophlebitis.
Signs of open
An open injury cannot be overlooked if blood flows out. Often this symptom is absent if the affected area is blocked by adjacent tissues or a blood clot. This violation provokes:
- drop in hemodynamics;
- severe pain;
- arterial bleeding.
The blood spreads quickly, forming hematomas. With extensive wounds, a state of shock is observed.
Arteries
When arterial networks are damaged, a scarlet stream leaves, the injured area hurts and goes numb. The skin becomes pale, gradually acquiring a cyanotic tint. There is increasing bruising at the affected area.
The muscles harden. There is difficulty in active movements with a gradual transition to passive contracture.
Ven
The main signs of injuries to venous vessels:
- bulging, bulging;
- swelling.
When wounded, dark liquor flows out in a stream. A small bruise without a pulse forms.
Although, there are no symptoms of ischemia with a vein contusion. The skin does not change color. Limb movements are not impaired.
A bruise is a rupture of a blood vessel
Bruise
- accumulation of blood in the subcutaneous fat, in body cavities or between layers of tissue, resulting from rupture of blood vessels and internal bleeding.
Bruise
- in forensic medicine, an area of surface tissue of the body, saturated with blood flowing out of a damaged vessel (vessels) under the pressure present in the cardiovascular system [1].
General characteristics [edit | edit code ]
It is customary to distinguish three main groups of bruises:
- actual bruising in the subcutaneous fat,
- hematomas (accumulation of blood between layers of tissue or in body cavities)
- petechiae (point intradermal or intraepithelial hemorrhages caused by ruptures of small vessels).
Actually, bruises are formed when exposed to a blunt traumatic object along a line perpendicular or almost perpendicular to the surface of the skin.
Mechanism of formation: impact, compression, stretching of tissues with blunt objects. When exposed to pressure, capillaries rupture; when stretched, larger vessels rupture (for example, bruises from cupping, Minakov spots, Vishnevsky spots, Tardieu spots). As a rule, bruises do not form on the abdomen and buttocks.
The shape and size of the bruise depend primarily on the volume of blood shed and the structural features of the fatty tissue at the site of impact. Mostly bruises have a round or oval shape. In extremely rare cases, a bruise may reflect the shape of the traumatic object.
Classification according to Solokhin-Bedrin [edit | edit code ]
- by origin: traumatic and pathological,
- by place of formation: local and distant (symptom of glasses),
- by time of appearance: early, late, very late,
- by depth: superficial, deep, very deep (subperiosteal),
- by size: petechiae, ecchymoses, large, hematomas,
- in shape: round, oval, rectangular, linear, etc.
"Blooming" of bruises [edit | edit code ]
In the first hours after its immediate formation, the bruise has a purplish-red color, which is caused by oxyhemoglobin. Then the transition of oxyhemoglobin to reduced hemoglobin occurs, and therefore the bruise changes its color to blue-violet with a purple tint.
Then, within 5 - 6 days, the breakdown of blood cells takes place and the subsequent transformation of hemoglobin into methemoglobin and verdochromogen, which has a green color. At this stage, the bruise takes on a greenish tint.
This is followed by the transformation of verdocromogen into biliverdin and bilirubin, which has a yellow color, as a result of which, 7 to 10 days after formation, the bruise acquires a yellowish tint.
Depending on the thickness of the bruise, changes in hemoglobin may occur unevenly, resulting in a color change from the periphery to the center of the bruise. After about 7 - 9 days, the bruise becomes three-colored: in the central part - blue-violet, along the periphery - yellow with a brownish tint, and in the intermediate zone - with a pronounced greenish tint.
The rate of color change depends on the size, location of the bruise, the age of the person and a number of other reasons. In some areas of the body, bruises never undergo the “blooming” process.
For example, bruises on the sclera of the eyes, after the formation of reduced hemoglobin and the acquisition of a blue-violet color, do not undergo further color changes. They gradually discolor, forming in their place areas of gray-yellow color, which can persist indefinitely.
Also, bruises located on the transitional border of the lips, the front surface of the neck, and nail beds are not subject to “blooming”.
bruise - bruise, and ... Russian spelling dictionary
bruise - bruise ... Dictionary of the use of the letter E
Bruising - Bruising is an accumulation of blood in the subcutaneous fat, in body cavities or between layers of tissue, resulting from rupture of blood vessels and internal bleeding. A bruise in forensic medicine is an area of surface tissue of the body, ... ... Wikipedia
bruise - bruise, bruises, bruise, bruises, bruise, bruises, bruise, bruises, bruise, bruises, bruises, bruises (Source: “Full accentuated paradigm according to A. A. Zaliznyak”) ... Forms of words
bruise - a; m. Subcutaneous hemorrhage, usually caused by a bruise, blow, etc. His whole body is covered in bruises: he was brutally beaten. * * * bruise (bruise), hemorrhage into soft tissue due to injury or without an external cause (for example, with hemorrhagic diathesis) ... Encyclopedic Dictionary
BLEEDING - BLEEDING, bruising, husband. Bruise from subcutaneous hemorrhage, usually caused by a bruise or blow. After the fight, his whole body was covered in bruises. Ushakov's explanatory dictionary. D.N. Ushakov. 1935 1940 ... Ushakov's Explanatory Dictionary
BLEEDING - BLEEDING, ah, husband. A bloody spot from subcutaneous hemorrhage after a bruise or blow. | adj. bleedy, oh, oh. Ozhegov's explanatory dictionary. S.I. Ozhegov, N.Yu. Shvedova. 1949 1992 ... Ozhegov's Explanatory Dictionary
Source: https://tkto.ru/krovopodtek-jeto-razryv-sosuda-sosudov/
Signs of closed
The peculiarity of closed damage is the direction from the inside to the outside. If the violation is minor from a blow with a blunt object, then a crack will form. The cerebrospinal fluid does not drain out, but a blood clot forms inside under the skin, which can cause ischemia.
With damage of the 2nd degree of severity, a circular intimal rupture is observed. An aneurysmal sac forms in the area of the aortic isthmus.
In severe cases, hemorrhages are extensive. They compress nearby tissues. This happens with a dislocation, a displaced fracture of a joint, or a severe sprain with a rupture. This type appears as:
- sharp pain that does not subside even after taking analgesics or straightening the bones;
- impairment of motor ability, sensitivity in the distal parts of the extremities;
- cyanosis, pallor, cyanosis;
- lack of pulse just below the injured area;
- the formation of an extensive hematoma when the integrity of all layers of the arterial walls is violated.
Clinical signs of injury
The danger of vascular injuries depends on the intensity and type of injury received.
Open
Open wound
Most often they manifest themselves in the form of external bleeding , but the vascular defect can be blocked by a blood clot or adjacent tissues, so in the presence of an open wound, sometimes there is no noticeable blood loss.
Injuries are also characterized by the passage of blood into soft tissues with the formation of a hematoma. Significant injuries lead to a drop in hemodynamics and the development of a state of shock. The most severe consequences are for arterial bleeding from large vessels.
Vascular injuries with open injuries come in three degrees of severity:
- Only the outer shell is damaged, the middle and inner layers are not affected.
- Through defect of the vascular wall.
- Complete rupture of an artery or vein.
Closed
With open injuries, the direction of injury goes from the outside to the inside, and with closed injuries it is the opposite, so the most severe cases are accompanied by complete destruction of the inner layer - the intima of the vessel. With minor injuries, cracks form in it. This is typical for impacts with blunt objects. There is no external bleeding, but an intravascular blood clot forms, leading to ischemia.
Formation of a blood clot due to a bruised vessel
The second degree of severity of closed vascular injuries occurs with a circular rupture of the intima and partially the middle layer. For example, in car accidents, a sharp impact leads to the formation of an aneurysmal sac in the area of the aortic isthmus. Severe injuries (third degree) are accompanied by extensive hemorrhages that compress the surrounding tissues. One option may be overextension with rupture due to a dislocated joint or a displaced fracture.
Symptoms of closed vascular injury:
- severe pain that does not decrease after the administration of painkillers or internal damage to the vessels of
bone reduction; - there is no pulse in the arteries below the area of injury;
- pale or bluish skin;
- extensive hematoma (when the vessel wall is destroyed).
Arteries
If a vessel from the arterial network is damaged, then there are the following characteristic signs:
- scarlet stream of blood;
- bleeding or rapidly growing hematoma with pulsation;
- There is no pulse in the arteries below the injury;
- pale skin, then cyanotic color;
- numbness;
- pain that does not decrease after fixing the limb does not increase when palpated;
- the muscles become hard (rigidity), initially active movements are difficult, and later passive movements are also difficult (contracture).
Ven
A wound to a venous vessel is manifested by a dark stream of blood, the limb swells, the peripheral veins overflow and swell, the blood stream is smooth. Formed hematomas are often small in size and do not pulsate. Unlike arterial bleeding, there are no signs of ischemia - there is a pulse in the artery, the skin is of normal color and temperature, movements in the limbs are possible (in the absence of a fracture or dislocation).
Vessels of the head and neck
Such injuries carry an increased risk to life. This is due to the following features:
- The respiratory tract and nerve plexuses are located close together, so respiratory arrest and reflex cessation of the heartbeat are possible;
- there is a threat of cessation of nutrition to brain tissue due to ischemia, thrombosis or air embolism with the development of stroke;
- abundant blood supply leads to large blood loss.
Brain contusion with damage to blood vessels
When an artery ruptures, there is severe bleeding or a hematoma forms with pulsation on the side of the neck. It quickly spreads to the area above the collarbone, puts pressure on the esophagus, and a breakthrough into the pleural cavity is possible. There is often damage (isolated or combined with arterial damage) to the vein. In this case, the accumulation of blood may not be noticeable; when palpating the neck, slight pulsation and swelling are noted.
Closed injuries are no less dangerous. Even light blows or manual therapy can cause dissection of the artery walls.
Severe pain occurs, disturbances in the blood supply to the brain with weakness in the limbs, slurred speech, facial asymmetry, and unsteady gait, which makes it possible to suspect a stroke.
Limbs
Signs of vessel rupture depend on its diameter and depth of injury. Large arterial and venous trunks pass through the limbs. Gushing bleeding from the femoral and brachial arteries is possible; due to the high speed, clots do not have time to form in them. In such cases, patients require emergency care to prevent major blood loss.
Closed fracture with vein damage
Blood flows out of a vein slowly, so most often blood clots form, but they can be washed away by the movement of blood. Venous bleeding is less intense, but it is not always possible to count on stopping it on its own. The most favorable option for vascular damage is capillary. In this case, the blood is similar to arterial blood, but the signs are only superficial, there is no ischemia.
If the blood clotting activity is normal, then such bleeding will stop when a bandage is applied.
Dangers
It is dangerous when large main vessels are injured. When infection, circulatory failure, or death of tissue cells occurs, gangrene can progress.
Another complication is multiple organ failure due to lack of oxygen, pathological changes in metabolism and impaired muscle nutrition.
In case of vascular defects, timely provision of first aid plays an important role. This will avoid a decrease in the performance of wounded areas of the body, and in some cases, save the life of the victim.
Possible consequences
The first group is fatal complications caused by collapse and hemorrhagic shock . The predominant localization is the great vessels and the heart:
- Left ventricle (we wrote about aneurysm of the left ventricle of the heart here);
- Aorta and its branches (read all the details about aortic aneurysm here);
- Pulmonary trunk (we talked about pulmonary aneurysm in more detail in this article).
The second group is complications that can lead to death , but more often cause ischemia and infarction of organs. Localization - internal organs:
- Brain (stroke);
- Renal arteries (kidney infarction);
- Intestinal vessels (peritonitis, intestinal obstruction).
The third group is peripheral complications . Ruptures in the area of the peripheral arteries lead to bleeding of the affected limb, followed by gangrene and amputation. If not diagnosed promptly, they can also cause death due to secondary infection.
Long-term consequences:
- Chronic renal, cardiac, liver failure;
- Decrease in intelligence and cognitive functions;
- Movement disorders, paralysis;
- Disorders of intestinal motility and urination.
First aid
Important actions in case of injury at the initial hospital stage.
- Apply ice to the affected area.
- Apply a pressure bandage if there is a rash.
- You can tighten it with a rope from clothing, or with your fingers, or a fist (if you don’t have anything at hand). The main thing is to squeeze it so that the blood does not flow out. For a child, wait 15-20 minutes, for an adult – up to 1 hour.
- Ensure immobility of the injured area. Do not warm, cool, or raise it.
If the neck area is affected, air bubbles may begin to enter and a brain embolism may occur. What to do with such damage to the walls of blood vessels? You need to apply a rolled bandage to the bleeding area. Raise the victim’s arm up and pass turns of the bandage through it along the second carotid artery.
In case of capillary injury, the area is treated with an antiseptic, a tight pressure bandage is applied, and a tourniquet is applied on top.
Be sure to remember the time for applying the bandage (no more than 1 hour). Otherwise, the blood supply will be severely disrupted.
If the internal arterial networks are disrupted, then it is worth applying a cold object to the chest or abdomen in order to achieve a spasm from the cold. In this case, you should not touch the patient. It’s better to get him to the hospital faster, but only in a horizontal position.
If the main networks are injured, then it is worth pinching the bleeding area (just above the wound) with your fist. Take the victim to the surgical department without delay.
Treatment methods
Treatment of conditions that develop due to a burst blood vessel in the brain is often symptomatic. Regulated risk factors are monitored. In cases where intracranial bleeding threatens serious complications, neurosurgical intervention is performed. Typically, surgery is prescribed if the diameter of the volumetric focus of hemorrhage exceeds 3 cm.
If the patient has undergone anticoagulant therapy, the drugs are discontinued and medications are prescribed that neutralize the effect - intravenous administration of blood plasma, prothrombin complex, vitamin K. The drug Dabigatran (anticoagulant) is eliminated through the hemodialysis procedure - extrarenal, hardware blood purification. The following events are taking place in parallel:
- Monitoring blood pressure levels (antihypertensive therapy with Nicardipine).
- Anticonvulsant therapy (if seizures are present).
- Mechanical ventilation (artificial ventilation) in case of depression of consciousness below 8 points (Glasgow coma scale), tachypnea 35-40 times per minute.
- Correction of hypoglycemia and hyperglycemia.
Early neurosurgical removal of large lobar (blood does not extend beyond the white matter) hematomas improves survival. However, surgical intervention is associated with the risk of relapse - repeated hemorrhage. The operation is not performed if the focus of hemorrhage is located in the deep parts of the brain.
Diagnosis and treatment
After the initial examination, patients are prescribed the following types of diagnostics:
- angiography to determine abnormal blood flow before scheduling surgery;
- a blood test in a laboratory to determine the degree of blood loss based on the level of hemoglobin, hematocrit, and red blood cells;
- Doppler ultrasound to obtain an assessment of the lumen of the arteries and the condition of their membranes;
- ;
- MRI.
The diagnosis is established based on the following criteria:
- pathological noises in the neck;
- reduction of pulsation;
- ischemic pain;
- contracture, muscle spasms;
- blood loss;
- tachycardia;
- increased thirst;
- darkening of the eyes.
The primary goal for venous arterial blood loss is to apply a pressure bandage or stop the bleeding. Emergency medical measures in a hospital setting:
- stopping bleeding;
- performing emergency surgery in life-threatening conditions;
- fasciotomy (surgical manipulation) for severe muscle swelling with subsequent excision of the defective area, autoplasty for aneurysms.
To restore the volume of circulating cerebrospinal fluid, patients are shown droppers with a solution of Albumin, glucose, and sodium chloride. In case of rupture of a large capillary, a transfusion of up to 2 liters is performed.
Diagnostics
The first choice methods for making a differential diagnosis are MRI and CT studies. Differentiation is made in relation to ischemic stroke and subarachnoid (intrathecal) hemorrhage. When making a diagnosis, it should be taken into account that acute neurological deficit can develop as a result of an epileptic seizure or hypoglycemia (a critical decrease in blood glucose levels). A blood test shows your glucose level. Computed tomography allows you to establish:
- Exact localization of the source of hemorrhage.
- Volume and prevalence of the pathological process.
- The presence and severity of cerebral edema.
- The presence and severity of dislocation of brain structures.
If MRI and CT examinations are not possible, a cerebrospinal fluid sample is taken as an alternative. Blood is detected in the cerebrospinal fluid if the focus of hemorrhage is in the area of the subarachnoid space or the posterior fossa of the skull. The attending physician will tell you what to do if a blood vessel in your head bursts, taking into account the results of the examination.
Forecast
It all depends on the type of damaged vessel and timely therapeutic actions. Of course, in case of capillary rupture, the prognosis is favorable.
The consequences of injuries to arteriovenous networks are more serious. Especially when limb ischemia begins, when the question of amputation is raised.
Purulent complications and decreased motor activity negatively affect a person’s labor prognosis. A big role is the correct application of a tourniquet, timely antibiotic therapy and rapid transportation of the patient to a specialized institution.
As a preventive measure, it is important to promptly identify and treat cardiac pathologies, strengthen vascular fibers, maintain a healthy lifestyle, and engage in sports.
The material was prepared specifically for the website venaprof.ru, edited by doctor E.Yu. Churilina. Specialty: dermatovenerology, general hygiene.
Surgery
After admission to the hospital, the patient first receives infusion therapy to restore circulating blood volume. For this purpose, droppers with isotonic solutions of sodium chloride, glucose, Albumin, Reopoliglucin, Voluven, Refortan are used. A blood transfusion of about 2 liters and 4 liters of solutions is indicated in case of damage to a large vessel.
Reconstructive surgery begins at a pressure of at least 100 mmHg. Art. and a pulse of about 100 beats per minute, but if the bleeding continues and threatens life, then the patient will be operated on immediately after hospitalization. Vascular operations are justified if there are signs of tissue viability - deep sensitivity is preserved, there is no muscle contracture. If these symptoms are present, the question of amputation is raised.
The integrity of the artery is restored in the following ways:
- side or circular seam;
- plastic surgery using your own vein or graft;
- connection of ends with a defect of no more than 2 cm.
If the vein is injured, a side suture is used, and if the damage is significant, then the femoral vein is isolated and used for plastic reconstruction.
First aid
The patient is isolated from others and the time of onset of symptoms is recorded. The patient should be moved only if absolutely necessary. In most cases, patients are unconscious. General algorithm:
- Gently shake the person by the shoulders and call - make sure there is no reaction;
- Call an ambulance;
- Provide access to fresh air;
- Free from outer, tight clothing, metal accessories;
- Check the airway (observe the chest, hold a mirror to your face);
- Feel the pulse in the arteries of the neck or wrist;
- If there is no breathing, begin cardiopulmonary resuscitation.
Resuscitation is carried out according to the following scheme:
- Thirty pressures on the chest area to a depth of 4-5 cm;
- Two breaths through the mouth (using gauze).
If the helper is not confident in his own skills, it is preferable to wait for the ambulance to arrive.
Diagnosis of aneurysm: examination and imaging methods
Diagnosis of aneurysms is made by a doctor through a physical examination: the doctor may feel the vessels in the abdomen or listen to noises caused by the flow of blood. Confirmation of the diagnosis is obtained using imaging techniques that photograph the bulge of the vessel and the presence of blood clots.
The most commonly used methods are:
- Ultrasonography . In which an image of the vessel is obtained by scanning tissue using ultrasound.
- Angio-MRI . This is a magnetic resonance technique that allows you to view images of blood vessels after the injection of an intravenous paramagnetic contrast agent.
- CT scan . Similar to an MRI, but the patient is given an intravenous contrast agent.