What is poor blood clotting?
Coagulation is a complex process of interaction between proteins, fibrins and platelets, which protects the individual’s body from significant blood loss due to injury. Under the influence of enzymes, substances are broken down and fibrin threads are formed in the blood. They have the ability to form blood clots that stop damage to small blood vessels. As a result, the bleeding stops. Blood coagulation in a healthy individual occurs with the formation of a blood clot within 10 minutes. Low coagulability is an abnormal process in which there is an enzymatic deficiency in the properties of fibrin.
This is a dangerous condition for an individual, and it is especially bad when poor blood clotting occurs during pregnancy. This phenomenon threatens the life of the expectant mother and fetus. With this pathology, there is a high probability of spontaneous miscarriage and large blood loss during delivery. It is very important to notice the occurring violations in time and assess their danger to the mother and baby. Planned studies help identify abnormal processes. Using the test results, the doctor will give recommendations and prescribe the necessary treatment that stabilizes blood clotting rates.
Disseminated intravascular coagulation syndrome (DIC syndrome)
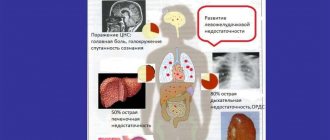
Disseminated intravascular coagulation syndrome (DIC) is a condition characterized by disturbances in the blood coagulation system.
In this case, depending on the stage of DIC, multiple thrombi (blood clots) form in the vessels of various organs or bleeding occurs. The blood coagulation system includes platelets and coagulation factors (specific proteins and inorganic substances). Normally, blood clotting mechanisms are activated when there is a defect in the vessel wall and bleeding. As a result, a thrombus (blood clot) forms, which clogs the damaged area. This protective mechanism prevents blood loss due to various injuries.
Disseminated intravascular coagulation syndrome occurs against the background of other serious diseases (for example, complications during childbirth and pregnancy, severe injuries, malignant tumors and others). At the same time, a significant amount of coagulation factors is released from damaged tissues, which leads to the formation of multiple blood clots in various organs and tissues. This impedes blood circulation in them and, as a result, causes their damage and dysfunction.
A large number of blood clots leads to a decrease in the number of blood clotting factors (they are consumed during the formation of blood clots). This reduces the blood's ability to clot and leads to bleeding (hypocoagulation stage).
DIC syndrome is a serious complication and threatens the patient's life. It is necessary to carry out urgent therapeutic measures aimed at treating the underlying disease (against the background of which DIC syndrome occurred), preventing the formation of new blood clots, stopping bleeding, restoring the deficiency of coagulation factors and blood components, and maintaining impaired body functions.
Consumption coagulopathy, defibration syndrome, thrombohemorrhagic syndrome.
Disseminated intravascular coagulation, consumption coagulopathy, defibration syndrome.
Symptoms of disseminated intravascular coagulation syndrome depend on the stage of the disease.
At the stage of increased blood clotting, multiple blood clots form in various organs.
With blood clots in the vessels of the heart and lungs, these and other symptoms may occur:
- chest pain (can spread to the left arm, shoulder, back, neck, jaw, upper abdomen);
- dyspnea;
- feeling of lack of air;
- cold sweat;
- nausea;
- vomit.
Signs of blood clots in the veins of the legs:
With thrombosis of cerebral vessels, acute cerebrovascular accident (stroke) can develop. He is accompanied by:
- headache;
- loss of consciousness;
- nausea, vomiting;
- speech disorders;
- muscle weakness or immobility of an arm or leg on one side;
- muscle weakness or immobility on one side of the face;
- numbness predominantly on one side of the body.
The formation of blood clots in the vessels of other organs (for example, kidneys) leads to their damage and dysfunction (renal failure).
The amount of blood clotting factors gradually decreases, as they are consumed in the process of forming multiple blood clots. As a result, DIC enters the stage of hypocoagulation (reduced blood clotting). This may cause bleeding.
Symptoms of internal bleeding (into various internal organs and tissues):
- blood in the urine - as a result of hemorrhage in the bladder, kidneys;
- blood in stool – bleeding in the gastrointestinal tract (for example, in the stomach, small intestine);
- severe headache, loss of consciousness, convulsions and other manifestations - with hemorrhage in the brain.
- prolonged bleeding even from minimal skin lesions (for example, from the injection site);
- bleeding from the nose, gums;
- prolonged heavy menstrual bleeding in women;
- pinpoint hemorrhages on the skin (petechiae).
Thus, the manifestations of disseminated intravascular coagulation syndrome are diverse and depend on the stage of DIC syndrome and the predominant damage to certain organs.
General information about the disease
Disseminated intravascular coagulation syndrome is a disorder in the blood coagulation system that develops against the background of various serious diseases.
The reasons for the development of DIC syndrome may be:
- complications during pregnancy and childbirth (for example, placental abruption, fetal death, severe blood loss and others);
- sepsis is a serious disease in which the infection circulates in the blood and spreads throughout the body;
- severe injuries, burns, in which a large amount of substances from destroyed cells enter the bloodstream, the endothelium (the inner wall of blood vessels) is damaged; these and other mechanisms can cause activation of blood coagulation processes;
- malignant tumors - the mechanism of development of disseminated intravascular coagulation in malignant tumors has not been fully studied; according to researchers, some types of malignant tumors (for example, pancreatic adenocarcinoma) can release substances into the blood that activate blood coagulation processes;
- Vascular disorders – vascular diseases such as aortic aneurysm (an enlargement of a vessel that threatens to rupture) can cause a local increase in coagulation (blood clotting). Once in the bloodstream, activated coagulation factors lead to disseminated intravascular coagulation throughout the body;
- poisonous snake bites.
Thus, these conditions can cause the release of a large number of blood clotting stimulants into the blood, resulting in the formation of blood clots in the vessels of various organs. This can lead to disruption of the blood supply to the lungs, kidneys, brain, liver and other organs. In the most severe cases, severe dysfunction of several organs occurs (multiple organ failure).
Gradually, the level of blood clotting factors decreases, as they are consumed during the formation of blood clots. As a result, the blood's ability to clot is sharply reduced. This may lead to bleeding. The severity of bleeding can vary from small hemorrhages on the skin (petechiae) to massive bleeding from the gastrointestinal tract, hemorrhages in the brain, lungs and other organs.
Disseminated intravascular coagulation syndrome can be acute or chronic. In acute DIC syndrome, after a short phase of hypercoagulation (increased blood clotting), hypocoagulation (decreased blood clotting) may develop. In this case, the main manifestations will be the occurrence of bleeding and hemorrhages in various organs.
In chronic DIC, the formation of blood clots comes to the fore. Cancer is a common cause of chronic disseminated intravascular coagulation syndrome.
Disseminated intravascular coagulation syndrome is a serious complication. According to various researchers, the presence of disseminated intravascular coagulation syndrome increases the risk of death by 1.5 - 2 times.
Who is at risk?
Risk groups include:
- women who have serious complications during pregnancy and childbirth (for example, placental abruption)
- patients with sepsis (a serious condition in which infection spreads through the bloodstream throughout the body)
- persons with severe injuries, burns
- persons with malignant tumors (for example, prostate adenocarcinoma)
- persons who have been bitten by poisonous snakes.
Symptoms of poor clotting
Signs of the disease may not manifest themselves for a long time. Over time, abnormal changes occurring in the blood coagulation system increase. The main symptoms of poor blood clotting during pregnancy are:
- Frequent multiple hematomas with minor physical impacts.
- Nosebleeds.
- Detection of red blood cells in urine.
- Bleeding when brushing teeth.
- The appearance of small wounds and cracks on the dermis without external influences.
Subsequently, anemia occurs, manifested by weakness, dizziness, hair loss, brittle nails, diarrhea and constipation. A characteristic feature is the pallor of the mucous membrane of the inner lower eyelid of the eyes.
The essence of pathology
Poor clotting is a dangerous pathology that threatens the life of the mother and the unborn baby. The disease has several names:
- thrombocytopenia – insufficient production of platelets;
- fibrinopenia – lack of fibrinogen for blood clotting;
- hemophilia - a hereditary factor plays a special role; the disease is mainly transmitted from the mother to boys; females are extremely rarely affected.
In a woman’s body, with the onset of pregnancy, all body systems are rebuilt, including the circulatory system. The suppressed immunity of the expectant mother provokes poor blood clotting during pregnancy. What does this condition mean for a woman and child? A woman in labor may experience early miscarriages, premature birth, or placental abruption in the later stages. With this pathology, the fetus does not receive enough nutrients for full development. At birth, he may suffer from hemophilia, underdevelopment of certain organs and mental retardation.
Blood clotting disorders in pregnant women. Complications and consequences
The balance between the coagulation and anticoagulation systems is maintained through the interaction of platelets, coagulation factors and the process of fibrinolysis. A disorder affecting any of these links can cause serious pregnancy complications. Among these complications, the most dangerous is DIC syndrome (disseminated intravascular coagulation). This syndrome develops due to activation of the coagulation system, on the one hand, and the fibrinolysis system, on the other. DIC syndrome in pregnant women can be caused by various reasons. Among them:
- premature placental abruption - separation of a normally located placenta before the birth of a child. In 80% of cases, this disease is accompanied by bleeding from the genital tract, sometimes a hematoma forms behind the placenta. Bleeding is associated with a decrease in plasma concentrations of coagulation factors, fibrinogen and platelets;
- Amniotic fluid embolism is a rare but dangerous complication that develops during complicated labor and is caused by the entry of amniotic fluid into the mother’s bloodstream and pulmonary vessels, which leads to acute respiratory failure and shock. DIC syndrome develops as a result of massive entry into the bloodstream of tissue thromboplastin, a substance that triggers the blood clotting process;
- endometritis - inflammation of the inner lining of the uterus - which develops after childbirth, can be complicated by the fulminant form of DIC syndrome.
Causes of poor clotting
Reduced levels of thrombocytopenia are uncommon in women. The main reasons for this phenomenon are:
- liver diseases - hepatitis, cirrhosis, which complicate the clotting factor;
- lack of vitamin K and calcium;
- acute and chronic leukemia;
- allergic reactions;
- congenital disorders of enzymatic connections between blood clotting factors;
- hemophilia - found to occur in rare cases in females;
- taking certain medications.
Blood clotting is also affected by prolonged bleeding, decreased immunity, and environmental conditions.
What are the dangers of poor blood clotting during pregnancy?
During pregnancy, all women undergo complex hormonal and immune changes in the functioning of the body. Fibronopenia occurs as a result of a disruption of the immune system, so that the mother’s body does not reject the developing fetus as a foreign body that has a different genetic protein structure. This phenomenon, due to its low viscosity, sometimes prevents the development of hemorrhoids, thrombophlebitis and varicose veins. But beyond a certain limit of decreased platelet levels, poor blood clotting during pregnancy causes complications. These include:
- Spontaneous termination of pregnancy in the early stages.
- Placental abruption.
- Premature delivery.
- Heavy bleeding during childbirth.
Prolonged bleeding, which cannot be stopped during obstetrics, leads to damage to the internal organs and joints of the woman in labor, disrupting the vital system. A reduced protective reaction results in a high percentage of death during childbirth. What is the risk of poor blood clotting during pregnancy for a child? Violation of the coagulation process in the maternal body causes an abnormality in the development of hemostasis in the fetus. After delivery, the baby may suffer:
- hemophilia;
- various forms of thrombocytopenia;
- abnormally formed organs;
- deviations in mental development.
The condition of thrombocytopenia necessarily requires correction, which is carried out by the attending doctor.
Hypercoagulability during pregnancy
During pregnancy, all women experience increased blood viscosity. As pregnancy progresses, the blood thickens more and more. This is how nature protects a woman from blood loss during childbirth and in the early postpartum period.
But it happens that the degree of blood thickening exceeds the maximum permissible values for pregnancy (hypercoagulation) and such “defense” begins to work as an “attack”, disrupting microcirculation in the implantation zone - the attachment of the fertilized egg (if we are talking about early stages) or in the uterine placental system (in terms of more than 14 weeks), causing malnutrition of the baby, which, if progressed, can lead to the most unfavorable pregnancy outcomes.
The group at increased risk of hypercoagulation during pregnancy includes women who have cardiovascular diseases, have previously suffered a pregnancy arrest at any stage, complications of past pregnancies such as gestosis, feto-placental insufficiency, premature placental abruption. During the examination at the stage of preparation for pregnancy, such women are often found to carry special gene variants that lead to a tendency to microcirculation disorders (mutations of hemostasis genes, https://www.cirlab.ru/price/538/). When such mutations are identified, a mandatory examination of the hemostatic system is carried out outside of provoking factors (pregnancy, taking hormonal drugs, etc.).
Based on the results, an appropriate regimen for taking “blood-thinning” drugs is selected at the stage of pregnancy planning and an action plan is developed when pregnancy occurs.
During pregnancy, such patients are monitored for the functioning of the blood coagulation system once every 4 weeks, even if “everything is normal.”
Very often, hypercoagulation is an incidental finding during pregnancy and is detected only during a routine examination. (It is worth knowing that https://www.cirlab.ru/price/563/ should be checked at least 3 times during pregnancy - upon registration, then at 22-24 weeks, then at 32-34 weeks).
And, sometimes, timely treatment can prevent a lot of problems with the baby’s development.
If a woman has to take “blood-thinning” drugs in injections during pregnancy, then control tests should be taken once every 2-3 weeks. Based on the results, the issue of correcting the scheme is decided.
Features of coagulation during pregnancy
During the normal course of pregnancy, from the second trimester there is an increase in the coagulation rate and a decrease in the anticoagulation system. In the blood of a woman expecting a baby, there is an increase in the level of fibrinogen in the blood plasma, a special protein that forms adhesive strings for the formation of a blood clot. And by the third trimester the reverse process begins. The blood thins when the production of platelets and their lifespan decrease.
Changes that occur when there are no other signs are normal and do not require correction of the condition. These changes after the birth of a child and rejection of the placenta protect the female body from significant blood loss. What are the risks of poor blood clotting during pregnancy? If it is impossible to quickly stop the bleeding, a woman loses a significant amount of it in a short period of time, which often causes death. Clotting problems often occur in the following category of females with:
- multiple pregnancy;
- hereditary predisposition;
- mental problems;
- Rhesus conflict;
- concomitant pathologies of the kidneys, endocrine system, blood vessels and heart.
In addition, problems with low blood clotting often occur in primiparous women after 40 and under 18 years of age.
Blood clotting disorders in pregnant women. Complications and consequences
The balance between the coagulation and anticoagulation systems is maintained through the interaction of platelets, coagulation factors and the process of fibrinolysis. A disorder affecting any of these links can cause serious pregnancy complications. Among these complications, the most dangerous is DIC syndrome (disseminated intravascular coagulation). This syndrome develops due to activation of the coagulation system, on the one hand, and the fibrinolysis system, on the other. DIC syndrome in pregnant women can be caused by various reasons. Among them:
- premature placental abruption - separation of a normally located placenta before the birth of a child. In 80% of cases, this disease is accompanied by bleeding from the genital tract, sometimes a hematoma forms behind the placenta. Bleeding is associated with a decrease in plasma concentrations of coagulation factors, fibrinogen and platelets;
- Amniotic fluid embolism is a rare but dangerous complication that develops during complicated labor and is caused by the entry of amniotic fluid into the mother’s bloodstream and pulmonary vessels, which leads to acute respiratory failure and shock. DIC syndrome develops as a result of massive entry into the bloodstream of tissue thromboplastin, a substance that triggers the blood clotting process;
- endometritis - inflammation of the inner lining of the uterus - which develops after childbirth, can be complicated by the fulminant form of DIC syndrome.
One of the reasons for termination of pregnancy at various stages is antiphospholipid syndrome (APS). APS is a complex of symptoms characterized by venous and arterial thrombosis. Pregnant women with antiphospholipid syndrome are at increased risk of miscarriage and spontaneous abortion due to a violation of the increase in the number of placental vessels with the development of fetoplacental insufficiency - a violation of the basic functions of the maternal placenta, leading to serious disturbances in the intrauterine development of the fetus, as well as due to vascular changes. To make a diagnosis of APS, in addition to increased thrombus formation, antibodies to phospholipids (the outer shell of membranes) are determined.
For medical questions, be sure to consult your doctor first
Diagnostics of deviations
During pregnancy, a routine examination of the woman in labor helps to determine that violations have occurred and poor blood clotting has occurred. Regularly, once every trimester, a laboratory test for coagulation is carried out and a coagulogram is issued, in which all indicators about the coagulation process are entered. The analysis is done more often if:
- surgery was performed;
- disorders associated with the immune system were detected;
- liver pathologies;
- vascular diseases are observed.
Particular attention is paid to the hereditary predisposition of a pregnant woman to coagulation disorders. Monitoring of the blood condition is intensified, and analysis is carried out more often than usual. This makes it possible to monitor the dynamics of deviations, the condition of the mother and fetus and allows you to take appropriate measures in a timely manner. If blood clotting is poor during pregnancy, the consequences for the child and mother can be very serious.
Decoding the coagulogram
The level of coagulation is determined by taking blood from a vein. The study is done on an empty stomach; the time interval between donating the biomaterial and eating should be at least eight hours. The coagulogram contains the following indicators:
- APTT shows the time it takes for blood clots to form. The norm is twenty seconds. If this indicator is lower, then the chances of blood clots are higher; if this indicator is higher, bleeding occurs.
- Fibrogen is a special protein involved in the formation of blood clots. At the end of pregnancy it is 6.5 g/l, it should not be more than this value.
- Platelets - synthesized by the bone marrow. The normal value is in the range of 131–402 thousand/µl.
- Lupus coagulant – shows antibodies. They shouldn't be normal at all. The presence of the indicator indicates the likelihood of miscarriage and thrombosis.
- Prothrombin is a plasma protein, the norm is from 78 to 142%.
All indicators are related to the duration of pregnancy and vary depending on the trimester and some other factors. If you receive the results of a bad test for blood clotting during pregnancy, you should not worry. It is deciphered by a doctor, and only he is able to correctly interpret the results.
Treatment
The choice of methods and means to eliminate hypercoagulation depends on the severity of the pathology, the duration of pregnancy, and the presence of concomitant or chronic diseases. Drug treatment is carried out until 36 weeks.
How to treat:
- Anticoagulants – Clexane, Cibor – reduce the risk of blood clots. The drugs are administered subcutaneously, the duration of therapy is at least 10 days.
- Antiplatelet agents – Curantil, Trental, Thrombo ACC. Improve microcirculation and uterine blood flow, prevent the development of fetoplacental insufficiency.
- Venotonics – Phlebodia. Prevent platelet aggregation and prevent the synthesis of free radicals.
- Vitamins E, C, P.
In severe cases, plasmapheresis and blood transfusion are performed.
Diet therapy must be prescribed. You can only eat boiled, stewed and steamed dishes, fermented milk products, seafood, seasonal vegetables and fruits.
It is necessary to completely exclude canned, smoked, fatty, fried foods, baked goods and sweets from the diet. You need to completely or partially give up salt.
The most useful products for preventing the development and eliminating hypercoagulation are sprouted wheat grains, corn, flaxseed and olive oil, citrus fruits, apples, red berries.
Treatment of poor clotting
After a routine examination of a pregnant woman, based on the results of a blood test and identifying the cause of poor coagulation, appropriate therapy is selected. There are nonspecific and specific treatments. The first includes the treatment of diseases that were acquired by a woman before pregnancy:
- Gastrointestinal tract - treats the digestive system.
- Liver - supportive treatment is prescribed.
- Pancreas – strict adherence to the diet is recommended: fatty, spicy and fried foods are excluded.
- Small intestine - it is very important to normalize its functioning, because the absorption of vitamin B12 and K, which affects blood clotting, occurs in the small intestine.
Specific treatment occurs using medications prescribed by the doctor, taking into account the individual characteristics of the woman’s body. How to treat poor blood clotting during pregnancy? For this use:
- Agents that enhance fibrinogen production – aminocaproic or tranexamic acid, “Contrical”.
- Indirect coagulants – “Vikasol”.
- Plasma transfusion improves clotting factors.
- Injection of fibrins obtained from donor blood.
Medicines prescribed by the doctor contribute to the normal bearing of the baby and reduce the chances of heavy bleeding during childbirth.
Why does thrombocytopenia occur?
Every woman should remember that it is imperative to plan a pregnancy, and to do this, undergo examinations by doctors even before conception, in order to be able to correct any changes in her body. What can cause poor blood clotting in pregnant women? There are several causes of this disease. If we talk about hereditary thrombocytopenia, expectant mothers who have:
- there are relatives who have had a stroke, heart attack, or thrombosis;
- there were varicose veins along the female line;
- the pregnancy was terminated naturally;
- there are disorders of the circulatory system.
An expectant mother can acquire thrombocytopenia:
- having had a viral infection;
- taking antibiotics;
- due to lack of vitamins;
- through intoxication;
- due to the consumption of products that contain preservatives or chemical additives.
Symptoms of poor blood clotting in an expectant mother
The main symptoms of thrombocytopenia in a pregnant woman will be:
- bleeding gums;
- the appearance of bruises on the body;
- frequent nosebleeds.
Treatment of thrombocytopenia
When a pregnant woman begins to notice any of the symptoms of poor blood clotting, she should immediately seek advice from her doctor. He, in turn, is obliged to refer the expectant mother to an appointment with a hematologist. Often, pregnant women are very frightened by any medications that they have to take while carrying a baby. Drugs that can normalize the circulatory system will not have a bad effect on the unborn child. On the contrary, they will help save the baby and also avoid severe bleeding during delivery. Many women wonder: is it possible to avoid thrombocytopenia during pregnancy? Of course available. To do this, it is necessary to strengthen blood vessels. In this case, folk recipes from nettle decoctions and rosehip tinctures will help. Lemons have a positive effect on blood composition. They must be consumed with the peel, adding honey. Citrine strengthens blood vessels; citrus fruits contain enough of it.
We also recommend reading: Low hemoglobin during pregnancy
Correction with products
After receiving a coagulogram, it turned out that there is poor blood clotting during pregnancy, what should I do? In case of minor deviations from the norm, the woman is advised to reconsider her diet, and medications may not be required. Listed below are foods that will improve coagulation. These include:
- milk-based products (high-fat cream and butter);
- liver, tongue, kidneys, heart;
- buckwheat porridge;
- pork meat;
- vegetables: bell pepper, red cabbage, boiled cabbage, turnip, radish, radish;
- greens: onion, dill, parsley, basil, garlic;
- legume grains;
- berries: mulberries, red and black currants, viburnum, blueberries, blackberries.
- fruits: banana, mango.
To improve the condition of poor blood clotting during pregnancy, drinking juice from white grapes and pomegranates, as well as walnuts, will help. It must be remembered that liquid thins the blood, so you need to control your drinking regime. Nutrition during pregnancy should be balanced and contain more vitamins and minerals. It is advisable to make all changes in diet only after consultation with your doctor.