Indicator norm
Pulse pressure is the difference between systolic and diastolic blood pressure, which is normally between 40 and 60 mmHg. The meaning is strictly individual, has gender and age differences, presented in the table.
| Age | PBP norms for women in mm Hg. Art. | PBP norms for men in mmHg. Art. |
| From 20 to 25 | 43 | 47 |
| From 25 to 30 | 44 | 51 |
| From 30 to 40 | 46 | 48 |
| From 40 to 60 | 52 | 51 |
| From 60 to 65 | 51 | 50 |
| Over 65 | 47 | 46 |
These are data from the EAC (European Association of Cardiology) based on the results of fifteen years of observation of several groups of patients. If deviations from the norm exceed 10 units, you should look for the cause of the pathological process developing in the body.
What indicators are considered normal?
Pulse pressure can normally fluctuate between 40-60 units. There is no general indicator, since this is an individual value for each person. The normal pulse pressure changes over the years. In youth, the PD value will be 40-45 units, in adults it is 50 points, and in adulthood it will reach 60 points.
The maximum value of pulse pressure is observed at 50-60 years of age, then the indicator decreases. Changes in PD are influenced by hormonal levels.
Table of pulse pressure by age:
| Age limits | Average PP for men | Average PD for women | Normal blood pressure indicators for men | Normal blood pressure indicators for women |
| 20 | 45 | 43 | 123/76 | 116/72 |
| 21-30 | 51 | 44 | 126/79 | 120/75 |
| 31-40 | 47 | 46 | 129/81 | 127/80 |
| 41-50 | 51 | 52 | 135/83 | 137/84 |
| 51-65 | 50 | 51 | 142/85 | 144/85 |
| Over 65 | 45 | 47 | 142/80 | 159/85 |
The table is compiled based on many years of research. Deviations from the table are permissible within minor limits.
Reasons for low PD
Low pulse pressure is said to occur when the difference between systolic and diastolic readings falls below 40 mmHg, which indicates serious problems with the heart (a fall of 25% from normal SBP threatens disaster). There are no physiological reasons for this condition. Hypothermia, stress, and physical activity cause slight fluctuations. Serious deviations from the norm have exclusively pathological causes. The main ones:
a – post-infarction large-focal cardiosclerosis; b – focal cardiosclerosis.
- bleeding, most often internal, causing hypovolemia: a drop in blood pressure reduces the pulse difference, as the body strives to compensate for discomfort and normalize tissue nutrition, but at the same time, the lack of nutrients significantly impairs the potential of internal organs;
- myocardial infarction, namely the left ventricle (acute disturbance of blood flow with the development of muscle necrosis) - leads to a sharp drop in PP to critical figures;
- cardiogenic shock - a consequence of a rapid drop in blood pressure due to aortic stenosis, AMI - can be fatal in a short time;
- decompensated heart failure creates a risk of spontaneous development of one of the fatal complications;
- inflammation of the heart muscle of various etiologies from myocarditis to pancarditis;
- hyperreninemia against the background of dysfunction of the hypothalamic-pituitary system, adrenal glands causes renal ischemia as a consequence of vascular spasm, a biochemical imbalance develops, causing a drop in pulse pressure, due to pathological regulation of vascular tone, impaired glomerular filtration, internal blood flow of the organ (prospective - chronic renal failure);
- atrophy of brain neurons with the development of encephalopathy, impaired control of vascular tone, and the formation of hypothalamic syndrome;
- vitamin deficiency, leading to profound changes in the nutrition of tissues and organs;
- various cardiovascular syndromes, for example, Morgagni-Adams-Stokes: a sharp decrease in cardiac blood output with the development of cerebral ischemia.
Understanding the causes of pathological fluctuations is necessary to prevent lethal complications.
How to calculate pulse pressure
Having learned what pulse pressure is, it is not difficult to calculate it yourself if you have a tonometer at hand. If you don’t have such a device in your home yet, you can go to a clinic or pharmacy where they can measure your blood pressure. Already at home, you can calculate what the difference is between the upper and lower indicators, receiving the current pulse pressure in numbers. For example, with a pressure of 130/90, the PAP is 40 mm, which is considered normal pulse pressure.
Patients ask doctors what pulse blood pressure reflects, if it is possible to use the upper and lower numbers, and they are probably enough to assess the condition of the heart and blood vessels.
The fact is that each of the indicators tells the doctor information about different organs. Previously, doctors believed that the most unfavorable condition was when diastolic pressure was higher than normal. The higher this indicator, the more obvious the risk of cardiovascular diseases, problems with the kidneys, thyroid gland, heart, blood vessels, etc.
On the other hand, an increase, reflecting the figures of systolic blood pressure, indicates the risk of heart failure, damage to blood vessels, myocardium, brain, and kidneys. Both numbers on the tonometer (upper and lower blood pressure) are considered integral, i.e. depending on many factors.
This is the frequency of contractions of the heart muscle, blood volume and viscosity, peripheral resistance of blood vessels, etc. Each of these factors is also multicomponent, therefore the difference between two indicators in the form of pulse pressure will also be integral, from which the doctor determines the condition of the heart muscle, arteries, etc. health parameters of organs and systems.
Reasons for high PP
Pulse pressure above 60 mmHg is considered to be high; it is caused by a number of reasons associated with disruption of the heart and blood vessels:
Stages of atherosclerosis: prelipid, lipoid, liposclerosis, atheromatosis, calcification
- hyperthermia, accompanied by hypertension with fluctuations in the upper and lower values;
- infections or autoimmune damage to the heart muscle;
- Alzheimer's disease;
- congenital or acquired heart defects, especially aortic valves;
- arterial hypertension of various etiologies, existing for a long time with a predominant increase in systolic pressure;
- decompensated renal failure;
- congestive heart failure, coronary heart disease;
- hyperfunction of the thyroid gland;
- atherosclerosis, which provokes narrowing of the lumen of blood vessels with atherosclerotic plaques;
- lack of vitamins;
- anemia;
- any pathology associated with disorders of the blood coagulation system, changes in its rheological properties;
- total vasospasm of various nature.
Other reasons are possible, including the formation of aneurysms of large vessels, changes in their course due to various pathological transformations.
Pulse pressure: what does this indicator mean?
Pulse pressure (PBP) is determined by subtracting the diastolic (lower) value from the systolic (upper) value after measuring blood pressure using a conventional tonometer.
On average, in a healthy person this number normally fluctuates in the range of 30-40 millimeters of mercury. Depends on the level of stroke volume of the heart and peripheral vascular resistance. As you can see, any person, using a mechanical or electronic tonometer, is able to measure his pulse pressure. This is a very informative integral indicator that allows you to draw numerous conclusions about the functioning of the heart and blood vessels. PAD reflects the following characteristics and features:
- functioning of cardiomyocytes;
- condition of blood vessels;
- volume of the heart ventricles;
- activity of chamber and aortic valves;
- atherosclerotic or inflammatory changes in heart tissue.
For a better assessment, PBP is measured at rest and after physical activity (it will be slightly higher).
This value is a good marker of hidden pathologies, since even with acceptable numbers of upper and lower pressure, PAP may deviate from the norm. That is why it is very important to constantly monitor this indicator.
Naturally, only a cardiologist can make the correct conclusion, so if you notice an underestimation or increase in this indicator, immediately contact a medical institution.
Symptoms of falling or increasing PP
Clinically, a drop in the difference between SBP and DBP is characteristic of hypotension, but a possible variant that occurs with a stable level of systolic and high diastolic pressure is isolated diastolic hypertension. High pulse pressure is formed against the background of long-standing hypertension and is associated mainly with fluctuations in the systolic rate. Symptoms of pathological fluctuations in men and women are presented in tables.
| Symptoms of falling PD | Symptoms of increased PD |
| Throbbing headache, often in the temporal region - a nonspecific symptom, reminiscent of migraine | Headache, usually in the back of the head |
| Lightheadedness, dizziness, loss of orientation in space | Nausea, vomiting caused by insufficient nutrition of the brain due to vascular spasm |
| Sweating, hypothermia due to disruption of the thermoregulation center | Hyperthermia, redness of the cheeks, hot flashes, redness of the facial skin - failure of the preoptic nucleus of the hypothalamus |
| Encephalopathy with ataxia (unsteady gait), orthostatic disorder | Vascular psychoses requiring correction in a special psychoneurological hospital |
| Cyanosis of the nasolabial triangle, shortness of breath | Speech disorders, slow movements |
| Loss of sensation in limbs | Paralysis, paresis |
| Drowsiness, apathy | Nervousness, tearfulness |
| Meteosensitivity | Meteor dependence |
| Bradycardia | Tachycardia |
This symptomatology may be accompanied by other nonspecific symptoms associated with vascular spasm or intoxication, but the main marker of the problem remains pulse pressure indicators.
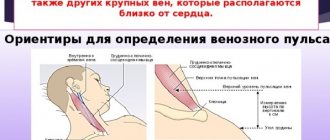
How to determine PD
It is often mistakenly believed that to determine PP it is necessary to count the pulse (it is more convenient to do this using a heart rate monitor), but in fact PP and heart rate are completely different indicators.
Determining pulse pressure and measuring pulse are not the same thing, they are different indicators
To determine PP, it is first necessary to measure blood pressure. Then make the calculation using the formula: PD = SD – DD, where:
- SD – systolic pressure;
- DD – diastolic pressure.
For example, a patient's blood pressure is 100/60 mmHg. Art. Accordingly, PP in this case will be equal to 40 mm Hg. Art. (100 – 60 = 40).
An increased PD is considered an even more dangerous condition than a decreased one. This is due to the fact that the higher it is, the harder the heart works.
Danger of pathology
Fluctuations in pulse pressure are dangerous for the development of fatal complications in men and women, such as:
- acute heart failure resulting in stroke or heart attack;
- chronic heart failure with symptoms of stagnation in the systemic and pulmonary circulation, dystrophy of internal organs;
- myocardial ischemia;
- pre-fainting, traumatic fainting;
- acute and chronic kidney failure;
- dementia, vascular psychoses, Alzheimer's disease;
- visual impairment.
To prevent such conditions, timely diagnosis and preventive treatment are needed.
Treatment
In acute conditions, therapy is always aimed at stopping the underlying disease (blood loss, renal ischemia, cardiogenic shock, and so on). As a rule, the drug complex includes drugs to increase the tone of the heart muscle (glycosides) - preparations of lily of the valley and foxglove are used. When blood volume decreases, plasma replacement solutions are indicated.
If the cause of the pathology is vasospasm, means are used to dilate them. These may be calcium channel blockers, myotropic antispasmodics, angiotensin antagonists or ACE inhibitors.
In cases where the cause of a sharp decrease in PP is stenosis or pathology of the aortic valves, or other severe disorders of the structure of the heart or its vessels, surgical treatment is indicated.
As for chronic conditions, therapy is aimed at maintaining vascular tone and normal blood pressure in general.
First aid
It is impossible to stop a large or small pulse difference on your own; an ambulance is needed. Before her arrival:
| With high blood pressure | At low pressure |
| Do not take any medications unless previously approved by your doctor | |
| Do not drink or eat anything (fainting, vomiting, aspiration of vomit), you can take sedative drops: Corvalol, Valocordin, Valerian | Eat something salty, drink a couple of glasses of water, a cup of coffee, green tea |
| Take a comfortable position, open the windows for oxygen flow, loosen tight clothes | |
| Carry out tonometry, record the results for the doctor | Tonometry every 10 minutes with accurate recording |
The doctor may suggest hospitalization, the patient has the right to refuse, but it is more reasonable to stop the attack inpatiently, under the supervision of specialists.
Treatment options
You should constantly monitor your pulse pressure, measure it 2 times a day. Remember that high or low blood pressure indicates the presence of a disease. You can purchase special mechanical and electronic blood pressure monitors in pharmacies. For frequent home use, it is recommended to purchase electronic blood pressure monitors, as they are convenient to use.
If a person discovers deviations from the norm of PD, then it is necessary to listen to the body. If there are no negative symptoms, and the pulse pressure quickly returns to normal, then you can limit yourself to the following measures:
- Systematic measurement of blood pressure and pressure;
- Making lifestyle changes (observe sleep patterns, increase physical activity, etc.);
- Eliminating bad habits.
If your health is disturbed, and PD indicators do not return to normal for a long period of time, you must immediately contact a specialist. Therapy, first of all, will consist of eliminating the cause that causes changes in PD indicators.
And since there are many such reasons, further treatment will differ. That is why it is strictly not recommended to self-medicate and prescribe medications on your own.
Diagnostics
The diagnostic algorithm for men and women is standard; after collecting an anamnesis, physical examination, and consultation with specialized specialists (if necessary), the following is carried out:
- tonometry with calculation of pulse difference;
- UAC, OAM, biochemistry;
- 24-hour blood pressure monitoring;
- ECG, EchoCG, cardio-ultrasound;
- Dopplerography of the vessels of the neck, head;
- blood testing for hormones;
- Ultrasound of the kidneys.
Additionally, any laboratory or instrumental examination may be prescribed to determine the cause of pathological fluctuations.
Drug treatment
Taking medications is an important part of treatment. Reducing the increased rate is achieved with the help of:
- Diuretics. These drugs remove excess fluid from the body and reduce the load on the heart, thereby reducing the risk of complications.
- Beta blockers. They are usually recommended for people who have had a heart attack. But they cannot be used in the presence of diabetes mellitus and dysfunction of the respiratory system.
- Calcium ion antagonists. Treatment is usually carried out with Isradipine or Nifedipine retard.
- Adenosine triphosphate inhibitors. They help restore the functioning of the nervous system and improve brain function.
During the treatment process, it is important to remember that you need to reduce blood pressure gradually. A sharp decrease can cause brain or kidney failure. Therefore, the listed and any other drugs should be prescribed by a doctor after a comprehensive examination and confirmation of the diagnosis.
Features of treatment
Deviations of normal blood pressure in any direction require identification of the root cause of the pathology and its elimination (relief). Without this, treatment is either useless or dangerous, since what helps with one disease can cause death in another.
Minor fluctuations in blood pressure do not require any intervention. They are most often one-time and physiological: temperature changes, climate zone changes, physical or psychological overload. The maximum that needs to be done is to consult a cardiologist in case of recurring abnormalities.
The doctor can prescribe folic acid - vitamin B9, which will support the heart and eliminate overload. The vitamin is produced by intestinal microflora and is responsible for cell growth and DNA preservation. During hyperloads, it is not enough, therefore, to stabilize the immune system, metabolic processes, and vascular elasticity, additional supply from the outside is necessary.
Patients with extra pounds and high pulse pressure are prescribed diuretics to normalize the total volume of circulating blood: from Furosemide, Diacarb, Hypothiazide to Triampur, Veroshpiron, Spironolactone. The treatment regimen is strictly individual, depending on the degree of obesity, blood pressure levels, and concomitant pathology.
In the presence of atherosclerosis, statins are added that normalize cholesterol metabolism: Atorvastatin, Rosuvastatin, Pitavastatin. They use nicotinic acid (niacin, vitamin PP, vitamin B) - a lipid-lowering agent, ion exchange resins (hemodialysis) or bile acid sequestrants: Cholestyramine, Colestipol, which reduce low-density lipoproteins that can destroy the arterial wall.
Age-related myocardial degeneration is stopped by prescribing cardiac glycosides: Digoxin, Celanide, Strophanthin. To reduce the diastolic index, Papaverine, calcium inhibitors: Amlodipine, Norvasc, Lacidipine, antispasmodics: Platiphylline, Scopolamine, Spazgan are prescribed.
To maintain vital functions, adrenergic drugs are used: Isadrin, Dobutamine, Dopamine. They act quickly, but only for a short time. For acute heart failure - intravenously - Amrinon and Milrinone.
Hormone replacement therapy can be used, and in extreme cases, surgical intervention: heart disease, aneurysms, total vascular atherosclerosis.
Reasons for deviation from the norm
Changes in the PP indicator are mainly a consequence of disturbances in the functioning of the cardiovascular system:
- Reduced elasticity of vascular walls due to atherosclerotic lesions, vasculitis of various origins (autoimmune, infectious, etc.), the presence of anomalies in the structure of large vessels (coarctation of the aorta or aneurysms of large vessels).
- Cardiac pathology, accompanied by myocardial hypertrophy or dilatation of cavities (insufficiency of the heart valve apparatus, aortic insufficiency, valve stenosis, myocardial infarction, etc.).
But besides this, changes in pulse pressure values can cause diseases of other organs and systems:
- Endocrinopathy. They mainly pay attention to the pathology of the thyroid gland, adrenal glands, gonads (thyrotoxicosis, pheochromocytoma, etc.).
- Hemoglobin deficiency of any origin (iron deficiency anemia, posthemorrhagic, hereditary thalassemia and other pathologies).
- Kidney diseases.
- Violations of vascular tone due to changes in autonomic regulation (VRR).
In children, the main cause of pulse pressure abnormalities is congenital heart defects and the consequences of previous infections.
In adolescence, VSD is recognized as the most common factor, since against the background of hormonal changes and puberty, there is a violation of the tone of the vascular walls and frequent changes in blood pressure.
Promotion
An increase in PP is most often observed with high systolic blood pressure. Normally, a slight increase within 10 units can occur after physical overload or emotional stress (for example, with a sudden fear). All this leads to the release into the blood of a large amount of adrenergic hormones (adrenaline and norepinephrine), which contribute to the contraction of the vascular wall, tachycardia and increased cardiac output against the background of a reduced stroke volume (the chambers of the heart do not have time to fill properly).
The main pathological cause of the increase is aortic insufficiency.
The symptom complex can occur in many diseases: congenital defects acquired against the background of autoimmune connective tissue diseases, the formation of atherosclerotic lesions, aneurysms, and so on.
Due to a violation of the elasticity and tone of the main vessel, a sharp decrease in diastolic pressure occurs against the background of increased systolic pressure, which is why a large difference and pulse hypertension is formed.
In old age, isolated arterial hypertension is a common cause. Most often, it occurs due to wear and tear of the walls of blood vessels with old age and a significant decrease in their elasticity and resistance. At the same time, systolic pressure increases, and diastolic pressure is within the normal range, forming a difference.
Demotion
The main reason for a decrease in pulse blood pressure is less than 20 mm. rt. Art. – a state of shock of various origins.
This difference leads to disruption of blood redistribution throughout the body and a decrease in cardiac output (possibly due to acute blood loss, cardiogenic shock due to myocardial infarction, acute heart failure, anaphylactic reaction, etc.).
Reflexively, circulatory failure leads to the activation of angiotensin mechanisms, which primarily affect the vascular bed, leveling collapse.
At the same time, vascular tone remains unchanged or even increases due to compensatory processes - in response to a stressful situation, a large number of hormones are released: adrenaline, norepinephrine, catecholamines, activation of the renal renin-angiotensin system and others, which contribute to the narrowing of the vascular wall and an increase in blood pressure.
Diastolic pressure increases due to increased vascular resistance, and systolic pressure decreases due to low filling of the left ventricle with blood.
Symptoms of the disease
A minor or single disturbance in heart rhythm may go unnoticed by a person and not cause discomfort.
But if the pulse deviates significantly from the norm, the following symptoms appear:
- irritability and inability to sleep;
- disruptions in the functioning of the cardiovascular system;
- feeling of weakness;
- difficulty breathing;
- decrease or increase in blood pressure;
- severe dizziness;
- cold sweat;
- nausea;
- poor concentration;
- fainting.
Bradycardia can be a serious health hazard . If the pulse reaches a critical level of 40 beats or below, then cardiac arrest is possible. Therefore, at the first signs, you need to ask yourself how to increase your low heart rate.
Treatment with medications is resorted to only in severe cases, in the presence of pronounced clinical manifestations. In all other cases, treatment at home is allowed.
Effective treatment
For timely diagnosis of diseases of the cardiovascular system, it is necessary to measure blood pressure twice a day. The measurement must be performed using a tonometer; at home it is convenient to use new electronic devices.
To normalize pulse pressure values, it is useful to perform light breathing exercises and use tonic medications. Among such remedies are tinctures of hawthorn and ginseng. However, you should not use such drugs without a prescription from a cardiologist. Self-medication can lead to irreversible consequences, including cardiac arrest.
This is influenced by stroke volume and vascular resistance. As people age, the walls of their arteries become stiffer. This increases the impulse pressure. High pulse pressure may be associated with reduced coronary perfusion. Therefore, it may be a predictor of future cardiovascular events, but this is not supported by meta-analysis.
Value is higher than normal
There are no drugs specifically aimed at reducing arterial stiffness. Treatment should be aimed at systolic and diastolic pressure, and not at reducing pulse pressure. Cardiovascular events are more likely in patients with high blood pressure, but low blood pressure may also increase the risk.
Blood pressure is a measure of how hard the blood presses against the walls of blood vessels during heart contraction. This parameter is one of the most important markers of human health. The upper indicator in tonometry, that is, measuring pressure, is called systolic pressure. The lower one is diastolic. The difference between them is the pulse pressure; normally it varies from 35 to 45 mmHg. Art. A larger or smaller gap between systole and diastole may indicate a dysfunction of the nervous system, heart and blood vessels.
Classically, a wide pulse pressure is a sign of aortic valve regurgitation, and a narrow pulse pressure is a sign of aortic stenosis. In the absence of valvular disease, high pulse pressure may be a sign of stiffness in the arterial walls and is a risk factor for coronary heart disease and myocardial infarction. Many studies have identified pulse pressure as a predictor for future cardiovascular events. In some cases, pulse pressure was a better predictor than other blood pressure parameters.
Low pulse pressure can be a physiological feature of a person or a symptom of a pathological process. At the same time, in medical practice there is a whole list of various diseases that lead to such deviations. Some of them are characterized by a benign course, while others indicate prolonged disturbances in the functioning of organs and systems and lead to the development of life-threatening conditions.
If pulse pressure predicts mortality, the question arises whether changes in pulse pressure will influence clinical outcomes. The systemic arterial circulation consists of a pulsatile pump, the left ventricle, and a distributive arterial network including the aorta, great arteries, and microcirculation. Because the pump is pulsating, the hemodynamic description of the systemic circulation can be considered in terms of mean and pulse pressure. Mean arterial pressure is determined by cardiac output and peripheral vascular resistance, and pulse pressure is the difference between systolic and diastolic blood pressure.
Normal blood pressure by age
| Age | Average systolic pressure readings | Average diastolic pressure readings | Average pulse pressure readings |
| 20 | 116-123 | 72-76 | 44-47 |
| 30 | 120-129 | 75-79 | 45-50 |
| 40 | 127-130 | 80-81 | 47-49 |
| 50 | 130-135 | 83-85 | 48-52 |
| 60 | 132-137 | 85-87 | 47-50 |
| 65 and older | 132-137 | 88-89 | 45-47 |
The magnitude of the pulsatile component of systemic arterial pressure is largely determined by the interaction between left ventricular volume and arterial system compliance, possibly with additional contributions from wave reflection. Pressure waves moving from the heart to the periphery may be subject to wave reflection. This is where the back-and-forth pressure wave is reflected back toward the heart, especially in areas where arterial circulation is constricted. The magnitude and clinical significance of wave reflection is a subject of some uncertainty.
Normally, in humans, the shock wave caused by contraction of the heart muscle causes resistance in the vascular wall and elastic recoil. If the vessels are not elastic enough, the speed of the pulse wave increases, and the difference between systolic and diastolic pressure decreases. Low pulse pressure is the most common problem among older people. With age, a smaller volume of blood begins to be ejected, and the walls of blood vessels become more rigid. The pulse wave no longer exerts the usual pressure on them, which leads to the appearance of a minimal difference between systole and diastole. The following signs indicate a decrease in the elasticity of blood vessels:
Compliance of arterial circulation is defined as an increase in contained volume in response to increased pressure and the result of the arteries being distensible. The degree of their distensibility varies throughout the circulation, which is highest in the proximal aorta, which therefore has the greatest correspondence in the arterial circulation.
The magnitude of the large artery compliance is a function of arterial geometry and arterial wall properties, primarily wall stiffness. In healthy young adults, the wall is not rigid and therefore does not “buffer” each left ventricular output. This limits the rise in systolic pressure and provides an additional pump to deliver blood flow during diastole. With aging and certain diseases, large arteries become stiffer and gradually less able to provide a "buffer" function.
- noise in ears;
- chilliness, constantly cold fingers and toes;
- fatigue;
- sensation of pressure in the temple area.
Attention!
Low pulse pressure in older people, which is accompanied by shortness of breath and chest pain, may indicate the development of heart failure. This condition requires a mandatory visit to a cardiologist.
This results in an increase in systolic blood pressure and a decrease in diastolic blood pressure, which increases pulse pressure. The acute response of large arterial walls to increased pressure is nonlinear. As blood pressure rises, the walls become stiffer. Therefore, increasing the average pressure will lead to an increase in stiffness and an increase in impulse pressure. Of middle age, the increase in pulse pressure largely depends on the degree of stiffness of the large arteries, while in young people it largely depends on the volume of cholesterol in the left ventricle.
The hereditary factor also plays a role. There is a high probability of developing low pulse pressure in people whose immediate relatives suffer from hypotension or neurocirculatory dystonia. Insufficient elasticity and increased tone of the vascular walls are factors that stimulate the formation of pathology.
In addition to aging, atherosclerosis increases the stiffness of large arteries. Thus, increased arterial stiffness may be a surrogate marker of atherosclerotic vascular disease. Extended pulse pressure may be a marker of the extent of coronary disease. Measurement of pulse wave velocity has been suggested as a useful adjunct to risk assessment.
Consequences of changes in pulse pressure
The physiological consequences of stiffened large arteries can be associated with both an increase in systolic blood pressure and a drop in diastolic blood pressure. Increases in systolic and pulse pressure can lead to further vascular damage and stiffness, creating a harmful feedback loop. Experimentally enhanced pressure cycling has been shown to result in accelerated vascular damage, increasing the likelihood of cyclic cause and effect, whereby the strengthened vessel results in increased pressure impulses and further vascular damage.
In addition, low pulse pressure in some patients develops under the influence of the following factors:
- incorrectly selected therapy in the treatment of hypertension, due to which the upper pressure decreases, but the lower remains the same;
- severe hypothermia - this usually results in a sharp decrease in systolic pressure;
- emotional stress;
- mental illnesses, especially panic attacks have a detrimental effect on pulse pressure;
- heavy physical activity;
- long stay in a stuffy, poorly ventilated room.
To improve the functioning of the heart and blood vessels, people with low pulse pressure should follow several recommendations:
- Stick to a daily routine, while allotting about eight hours for sleep.
- Play sports outside, jogging or race walking. This measure helps to increase the contractility of the heart muscle.
- Regularly ventilate living and working areas.
- Try to minimize the amount of negative emotions and stress.
- Take vitamins A, E and preparations containing Omega-3 fatty acids.
Treatment for high and low blood pressure
When pulse pressure rises, folic acid helps reduce it. The effect of this vitamin is due to the fact that it reduces the level of homocysteine and cholesterol in the blood, thereby reducing the load on the heart. For hypertension, it is necessary to take beta blockers, which reduce systolic pressure by reducing cardiac output. Pulse pressure decreases with a decrease or normalization of body weight in obese people, as well as with the use of diuretics. Diuretics reduce the volume of circulating blood, and accordingly, the load on the heart decreases. To mitigate the manifestations of atherosclerosis, cholesterol-lowering drugs are used: statins, nicotinic acid, fibrates, ion exchange resins.
When pulse pressure decreases, help will be provided by drugs that increase myocardial tone - digitalis and lily of the valley glycosides. Hypovolemia requires an increase in the volume of circulating blood; for this, plasma-substituting solutions are administered intravenously. Diastolic pressure is reduced by drugs that dilate blood vessels. This is a group of calcium blockers, myotropic antispasmodics (Papaverine, Drotaverine), ACE inhibitors, angiotensin receptor antagonists. Treatment of kidney disease will help normalize DBP and PBP by reducing ischemia and renin production.
In case of defects of the aortic orifice and valve, surgical intervention is necessary - plastic surgery of the aortic valve or restoration of the patency of the orifice.
Contact a cardiologist if there is discomfort in the heart and changes in blood pressure.