Interruptions in the functioning of the heart occur not only in sick people. Scientists have proven that it beats with different intensities throughout the day, so you shouldn’t worry about this when identifying one-time symptoms. It’s another matter if these symptoms become frequent during the day and for a long period of time. Many heart diseases are passed down and are considered to run in families. If there is an organ dysfunction, it is important to know whether your loved ones suffer from the same problems. Below in the article are the symptoms, causes and types of abnormal heart rhythms.
Thoughts are material: psychosomatic arrhythmia due to nervousness during stress
Our readers successfully use ReCardio to treat hypertension.
Seeing how popular this product is, we decided to bring it to your attention. Read more here... In modern realities, it is difficult to live a day without experiencing stress at work or at home. Because of this, a person may develop heart rhythm disturbances. Common deviations: tachycardia and extrasystoles during neurosis have their own characteristics and methods of treatment.
What causes nervous arrhythmia?
In a normal state, a person’s various organs function harmoniously, the most important of which is the heart. By pulsating, it pumps blood throughout the body, enriching other organs with oxygen.
In a calm state, a healthy person has a normal heart rate, which increases with physical activity. If a person has tachycardia (a form of heart rhythm disturbance), then an increase in rhythm is observed regardless of the influence of external factors.
Important! Even an absolutely healthy person experiences several irregular contractions a day that he is not able to notice.
The causes of tachycardia are different. It is caused by diseases of the cardiovascular system, in which blood circulation is disrupted, which poses a threat to other organs. Disturbances in the rhythm of contractions are possible in stressful situations.
When a person experiences a strong shock (especially fear), he may feel a strong heartbeat, as if it would jump out of his chest.
But if such situations arise rarely, even in the case of frequent stressful situations, then there is no need to worry about rhythm disturbances. Arrhythmia can be considered neurological when even the slightest stress causes fluttering in the chest.
You can trace the connection between the psychological state and heart rate in a simple way. If you diagnose the pulse in a state of emotional rest, you can see how it quickens with a feeling of joy or negative emotions.
From this we can conclude that for normal well-being it is important that the heart functions at a moderate rhythm, regardless of the emotional state. Of course, it is pleasant to feel joy accompanied by a gentle beating in the chest, but in extreme situations such a violation can aggravate a person’s situation.
A heart rate in the range of 60-80 beats per minute is considered a normal rhythm. To check the rhythm, you can use a blood pressure monitor or count your pulse over a certain period of time.
Neurological arrhythmia is classified as follows:
- Tachycardia. In this case, during emotional shocks, the rhythm becomes more frequent (more than 80 beats per minute).
- Bradycardia. The rhythm slows down (less than 60 beats per minute).
- Extrasystole. With this pathology, the rhythm does not change, but from time to time extraordinary contractions appear that deviate from the general rhythm.
Psychosomatic symptoms
Psychosomatic cardiac arrhythmia has the same symptoms as other types of this disease. In most cases, abnormalities can be detected even without the participation of a doctor. Here are the signs that indicate this disease:
- Arrhythmic pulse at the wrist.
- Blood pressure surges.
To definitively establish arrhythmia, doctors perform electrocardiography.
First of all, we note that the symptoms of nervous arrhythmia have their own characteristics. This phenomenon cannot be considered a disease, although it is pathological, since rhythm changes appear under the influence of the emotional state, and not deviations in health.
The following symptoms confirming a psychosomatic rhythm disorder can be noted:
- Rhythm reaction even to minor emotions and at the moment of disturbing thoughts. Most often, periods of rhythm disturbance occur after waking up or before falling asleep.
- A sudden fear or surprise can cause sudden increases in heart rate. For example, if you mention any disease, the patient gets scared and his pulse quickens to 140-160.
- In half of the cases, there is a violation of the perception of reality. For example, a tonometer or ECG does not detect rhythm disturbances, but a person feels that he has a rapid heartbeat. In some situations, a slow pulse is observed, despite the fact that the patient speaks of tachycardia.
- Sudden feeling of fear. Due to a rapid heartbeat, the patient may have a fear of death, as a result of which the pulse increases even more.
- Other external factors. Often a change in pulse is observed with hot or cold flashes; numbness and trembling of the limbs can cause an accelerated heartbeat.
When examined by a doctor, patients with nervous arrhythmia can vividly talk about their symptoms and rhythm disturbances, dwelling on details and actively gesticulating. This is explained by the fact that they experience constant stress, including the fear of stress, which causes intense emotionality even in people who do not have this trait. Note that among patients with nervous rhythm disturbances, the majority are melancholic.
Some patients complain that they have moments of cardiac arrest that cannot be detected within a few minutes. Even this can cause stress, despite the absence of other serious symptoms.
Attention! Some patients have persistent tachycardia that does not respond even to a serious dose of antiarrhythmic drugs. Normalization of the rhythm occurs only after a person feels safe.
This is a rather complex diagnosis, because it is not always possible to establish the causes of rhythm disturbances. Diagnosing nervous rhythm disturbances becomes difficult because it requires rejecting all possible other factors.
Treatment of arrhythmia
The first step is to inform the patient that the cause of his problems is psychosomatics, and with this diagnosis there is no threat to health, because all changes in the rhythm are caused by his own fears. Having understood and realized this, the patient is able to reconsider his attitude towards rhythm disturbances and take measures to lead a fearless life.
But in no case should the complaints of a patient with a psychosomatic illness be dismissed, because if fear and stress persist, the quality of life will deteriorate.
Main rules of therapy
Stress arrhythmia refers to psychogenic illnesses, and not problems with the cardiovascular system. Therefore, methods of treating the disease against the background of stress are chosen accordingly. Antiarrhythmic drugs can be replaced with antidepressants to eliminate the patient's feelings of discomfort and anxiety. To get rid of stress, the patient needs to act as follows:
- Work with a psychotherapist. This is important even if finances are limited or the patient’s life principles do not allow the psychotherapist to interfere with his “brain”. Some patients may consider that spending money on eliminating psychosomatic tachycardia or bradycardia is unnecessary, since this is not a disease. But it's not just surgeons and other practitioners who treat serious illnesses. There is no point in depriving psychotherapists of their well-deserved praise.
- Change your lifestyle. Changes in everyday life will help you learn something new, overcome your fears and improve your emotional state. It is recommended to play sports to dispel illusions about your illness. With the help of exercises in the gym or pool, the patient will understand that his ailments have no physiological basis, and all the discomfort comes only from uncertainty.
- Avoid stress and look at life positively. At the same time, it is recommended to restore order not only in the mind, but also in life. You can clean out your closet or workplace so that your thoughts are appropriate. If after several days there is no improvement in your well-being, then you can return to your previous creative disorder. In addition, it is important to filter the information received every day. Don't burden yourself with unnecessary problems. It is important to be able to prioritize when completing multiple tasks. This will allow you to avoid unpleasant situations when there is not enough time to solve everything.
- To refuse from bad habits. Some will not be able to completely stop drinking or smoking, so you may wish them to at least minimize negative factors. The point of giving up bad habits is to not be dependent on anything. When you cannot satisfy your needs, a person involuntarily feels a deterioration in his mood.
How to recognize extrasystole during panic attacks?
The clinical picture is accompanied by the appearance of neurotic conditions, as well as the development of hypochondriacal disorders, which are characterized by:
- Interruptions in heart function in the morning and severe dizziness.
- Prolonged insomnia that occurs against the background of painful thoughts.
- Chills, fever and shortness of breath.
- Trembling hands, anxiety, nausea and restlessness.
- Fatigue and memory impairment.
- Feelings of nervousness, unreality and stiffness.
- Difficulty concentrating and fears.
In rare cases, a transition from extrasystole to tachycardia occurs. At the same time, the heart rate increases to 140-160 beats/min. This condition can develop even when mentioning a heart attack or angina. The symptoms of tachycardia may increase with somatic disorders, depressive cyclothymia, which are characterized by unstable mood.
Despite this, extrasystoles during panic attacks do not cause pathological changes in the heart. Excessive heartbeat is a natural reaction of the nervous and cardiovascular systems.
Bradycardia
Bradycardia is a heart rhythm disorder in which the heart rate decreases. In this case, the intervals between heart contractions remain constant. Bradycardia is a condition in which the heart rate is less than 60 beats per minute.
Manifestations of bradycardia: dizziness, weakness, fatigue, chest pain. It is difficult for a person to do physical work; it is difficult for him to concentrate on anything. It becomes difficult to breathe, shortness of breath appears, and fainting is possible. Blood pressure is reduced.
However, it happens that bradycardia does not manifest itself in any way.
Normally, the heart beats 60-80 times per minute. This occurs under the influence of impulses that generate special myocardial cells. These cells are found unevenly throughout the myocardium, but are grouped into several pacemakers. The main one is the first order pacemaker – the sinus node. It is located in the right atrium. Second-order pacemakers - the atrioventricular node, the His bundle and Purkinje fibers - conduct impulses throughout the myocardium. That is, the heart contracts gradually, but since this happens very quickly, in a split second, the time difference between the contraction of, for example, the right atrium and the left ventricle is almost imperceptible.
However, as a result of any violations, impulses can be generated either too often, then they speak of tachycardia, or too rarely, then they speak of bradycardia. Both tachycardia and bradycardia are not independent diseases, but symptoms.
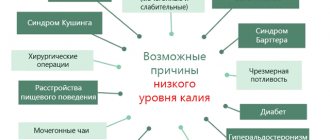
Bradycardia can develop as a result of:
In some cases, bradycardia develops during prolonged standing, pain, coughing, and vomiting.
In athletes, the heart rate is often less than 60 beats per minute. This happens because the heart learns as a result of long-term training to work at full strength, and even that small number of contractions for an ordinary person is enough to supply blood to all organs and tissues. Bradycardia is also possible in people with a naturally “strong” heart.
Bradycardia is dangerous because, as a result of too rare heart contractions, a sufficient amount of oxygen does not reach the organs and tissues. And oxygen deprivation can cause not only fainting, but also injuries resulting from this fainting.
Diagnostics
To diagnose bradycardia, you need to be examined by a therapist and a cardiologist. You also need to take a general blood test, a biochemical blood test, and a test for thyroid hormones. You definitely need to do an electrocardiogram.
To determine the cause of bradycardia, data from Holter cardiac monitoring, a stress test, and orthostatic tests are needed.
In some cases, a log of identified symptoms may be needed. The patient should write down the symptoms and the activities he was doing when the symptom appeared. This log is usually kept in conjunction with Holter monitoring.
Treatment of bradycardia most often involves treating the underlying disease. That is, in case of hypothyroidism, the necessary hormones are prescribed, and in case of electrolyte imbalance, appropriate medications are prescribed. If bradycardia is caused by medications, then, at the discretion of the doctor, you need to either replace this drug or simply reduce the dosage.
In some cases, bradycardia requires a pacemaker. It is needed if the sinus node is malfunctioning or impulses do not pass between the atria and ventricles.
Lifestyle
A patient with a pacemaker should regularly measure their pulse rate, undergo regular medical examinations, and regularly report data on the operation of the pacemaker to the doctor. Typically, the battery of this device lasts for 5-15 years.
Household electrical appliances do not affect the operation of the pacemaker, since they have a weak electromagnetic field. However, patients with a pacemaker cannot operate industrial electrical equipment. Be careful around strong magnets and magnetic detectors, such as those found at airports, arc welding machines, and industrial power generators. Such patients should not walk near power lines or be near amateur radios. They cannot undergo magnetic resonance imaging. However, CT scanning is safe for such patients.
Prevention
To prevent bradycardia, doctors recommend exercising and staying in good physical shape, quitting smoking, eating right, and monitoring blood pressure and cholesterol levels. It is very important to maintain a normal weight and also avoid stress.
Neurogenic bradycardia
Neurogenic bradycardia is a symptomatic pathology that develops against the background of extracardiac diseases. If the underlying disease does not pose a threat to human health, then there is no need to worry about long-term consequences. The only thing is that it is important to carry out the correct treatment from the very beginning.
Bradycardia is defined as a heart rate below 60 beats/min in adults. In children, heart rate is determined depending on age, for example, up to a year, a decrease in heart rate below 110 beats/min is considered abnormal.
In the diagnostic process, standard methods are used, primarily electrocardiography. Additionally, laboratory tests, stress tests, ultrasound of the heart, as well as specific research methods are performed that will help determine the exact cause of the pathological condition.
Video Bradycardia | What to do
Description of neurogenic bradycardia
During the development of the pathological condition, the following forms of slow rhythm can be observed: sinus and non-sinus. The latter type is characterized by the formation of a blockade of impulse conduction, therefore such a rhythm disturbance in clinical practice is considered implicit bradycardia.
Sinus bradycardia is characterized by decreased activity of the sinus node. This form often develops against the background of various autonomic disorders, especially with increased tone of the parasympathetic nervous system. If disorders of other organs and systems are observed, then sinoauricular conduction disturbance may occur.
Symptoms of neurogenic bradycardia
The development of bradycardia can be determined by such signs as increased fatigue, a pronounced feeling of weakness, lack of attention and memory loss. The patient also begins to cope worse with usual responsibilities, and in some cases it becomes difficult to perform physical exercises.
Moderate and minor bradycardia, as a rule, does not cause hemodynamic disturbances, as a result of which the clinical picture of these conditions is poorly expressed.
Depending on the underlying disease, the following symptoms may be observed:
- cold sweat;
- pain in the heart area;
- sudden jumps in blood pressure;
- difficulty breathing;
- minor visual disturbances.
During an attack, various periods of slowing contractility can be observed. If you experience severe anxiety, sudden dizziness, or fainting, then you should immediately consult a doctor.
Causes of neurogenic bradycardia
The development of pathology often involves various pathological conditions not associated with diseases of the heart and blood vessels. Most often, neurogenic bradycardia occurs against the background of the following pathologies:
- Neurosis-like conditions, which are characterized by a chronic course and the predominance of psychogenic factors of influence.
- Vagoinsular crises associated with a disorder of the autonomic nervous system.
- Bleeding into the subarachnoid space, often due to traumatic brain injury.
- Inflammation of the labyrinth in the inner ear.
- Colic of various origins (hepatic, renal, intestinal).
- Peptic ulcers of the stomach and duodenum.
- Hiatal hernia.
- Reflex reactions affecting cardiac activity (severe hypothermia, severe pain).
- Convalescence carried out after severe protracted illnesses.
When is treatment needed?
In order to get rid of extrasystole during panic attacks, it is recommended to take measures to eliminate the underlying causes. The first thing you need to do is visit a doctor to diagnose and treat anxiety disorders of the neurotic level that arise due to stress. Please note that panic attacks can also act not as an underlying disease, but as a symptom of rheumatic disease, mental, cardiovascular and endocrine pathologies. That is why, when extrasystole appears, doctors prescribe a comprehensive diagnosis, which makes it possible to establish the true cause of the heart rhythm disturbance.
Midazolam injections are prescribed for panic attacks
For the medical treatment of a panic attack, it is recommended to use the following drugs:
- "Diazepam." It has a pronounced anti-anxiety and sedative effect. 5 mg is administered intramuscularly. If there is such a need, the injection is repeated.
- "Midazolam." It has a hypnotic and anti-panic effect. 3 ml is administered intramuscularly. The effect of the injection is achieved after 10 minutes.
- "Temazepam." The drug eliminates tension and calms, relieving a panic attack. Take 2 tablets orally.
In order to improve the general condition of the patient, sedatives are prescribed. Thus, it is possible to increase sensitivity and transfer the reaction to the level of the subcortex, which significantly reduces the perception of extrasystole by the consciousness. This approach improves the perception of ongoing interruptions, making them less noticeable.
If a person with extrasystole goes to a cardiologist, then first of all drugs such as “Propanorm” and “Citalex” are prescribed. Many doctors believe that such treatment is unacceptable, since these medications can worsen the course of panic attacks, and thereby aggravate extrasystoles.
Diagnosis of neurogenic bradycardia
During a medical examination of a patient with neurogenic bradycardia, the percentage of decrease in heart rate is determined. To clarify the diagnosis, electrocardiography is required, which detects the following changes:
- intact P wave with normal atrioventricular conduction (corresponds to sinus arrhythmia);
- decrease in heart rate.
Holter monitoring helps to clarify the diagnosis. With its help, an ECG is recorded over the course of a day or two, after which the data is analyzed for the presence of subtle rhythm disturbances. If the underlying disease is associated with hormonal disorders or disorders of the gastrointestinal tract and other organs other than the heart, then diagnostic methods such as laboratory tests are used.
And here is what antiarrhythmologist Alexander Ivanovich Korzun says about extrasystole:
“ extrasystole and does not require treatment. To their misfortune, someone feels these extrasystoles. In such cases, it is optimal to distract yourself with life: friends, family, children, work, hobbies, etc. If you can’t get distracted, then you need the help of a psychotherapist.”
According to these experienced doctors, it turns out that it does not matter what kind of extrasystoles a person has: ventricular, supraventricular, or preventricular. It is important that if he does not have organic heart disease, then the problem of extrasystole can be successfully solved with the help of a psychotherapist. There are also good experts who say: before there was no holder, and all people lived peacefully. Now the problem arises due to the fact that a person begins to feel extrasystoles, and the holder records them, thus creating a problem. Psychotherapy helps here, that is, increasing stress resistance.
True, the same Korzun also says that extrasystole is often a consequence of problems of the gastrointestinal tract. And gastrointestinal diseases primarily occur in people suffering from nervous disorders. Therefore, if a person really has problems with the gastrointestinal tract (gastritis, ulcers, reflux esophagitis), then he really needs to first treat the stomach in order to reduce the severity and manifestations of extrasystoles.
About drugs
Often, if a person goes to a cardiologist, he is prescribed antiarrhythmic drugs: Citalex, Propanorm, etc. Here, everyone takes responsibility for themselves whether they will take these medications or not, but reliable sources say that these drugs worsen a person’s condition. Therefore, you just need to keep in mind that with a healthy heart, extrasystole does not cause any problems. Problems begin when a person begins to obsess over them, when he begins to struggle with them, when he begins to read what he does not need to read and interpret it incorrectly.
With all the trust and respect for Eduard Guglin or Alexander Korzun, by constantly visiting their sites, a person only harms himself because he comes across some messages that he does not need. He begins to read about other types of arrhythmia, about other problems, without understanding the connection between them and taking individual phrases out of context.
Simply because an ordinary person who has problems and is looking for solutions to them is not a qualified cardiologist.
Therefore, if a person has such a symptom of vegetative-vascular dystonia as extrasystole , and he really wants to get rid of this problem, then, first of all, it is necessary to exclude communication on this topic, stop visiting medical sites and begin to move along the path of getting rid of neurosis, from anxiety disorder, from your internal tension, which leads to these problems. And then the extrasystole will gradually go away.
Of course, this article is intended for a rather narrow audience: some have extrasystole , others do not. If you don't have one, you're lucky: you don't even have to think that you might have one. But if it does appear, you are doubly lucky, because you will know that this is a completely harmless form of arrhythmia.
Treatment and prevention of neurogenic bradycardia
Specific therapy is carried out only if a severe pathology is determined. Depending on the severity of the process, treatment can be prescribed on an outpatient basis or carried out in a specialized cardiology department.
Commonly used treatments for neurogenic bradycardia:
- Drug therapy is aimed at eliminating the underlying disease, for which appropriate medications are prescribed. To eliminate the symptoms of a slow rhythm, medications such as alupenta, atropine, and isadrin are used. If there are contraindications to the last two drugs, then ipratropium ephedrine is used.
- Surgical treatment is carried out as a last resort when the patient is not helped by medications or there are serious contraindications to taking them. As a result, the patient is prescribed a pacemaker implantation, which helps prevent sudden cardiac arrest.
When carrying out prevention, the following recommendations should be taken into account:
- absence of bad habits such as drinking alcohol and smoking;
- properly planned daily routine;
- nutritious nutrition containing heart-healthy foods;
- carrying out therapeutic measures to eliminate concomitant diseases;
- You should take medications only after medical consultation.
Bradycardia with VSD - what should you be wary of?
“You won’t please us!”
– dystonics joke about their problems. Indeed, as soon as the heart accelerates to 90-100, panic begins, even though the doctors would not have seen anything critical. The VSD worker behaves as if his heart is about to burst. But the other side of the problem is no less frightening, especially since bradycardia with VSD occurs less frequently than tachycardia. And the patient, confident that his heart muscle can stop at any moment, is afraid to go to bed. The usual lifestyle on the couch or in front of the monitor also becomes difficult due to a low pulse. Moreover, with neurocirculatory dysfunction, accompanied by eternal hypochondria, a person acutely feels the work of almost every organ. Instantly detects all problems. Especially when it comes to the heart, whose work is actually “present.” At any moment we can listen and feel its rhythm, or place our fingers on the pulsating wrist. Is low pulse dangerous with vegetative-vascular dystonia?
How to overcome heart pain and cope with fear during VSD
Pain due to VSD is treated not only by neurologists. This disease has recently been classified as a psychiatric disease, so psychologists are coming to help with recovery. The treatment is based on working with a person’s mental state; it is necessary to rid the patient of panic attacks and teach him how to relax correctly.
An important factor for the patient is the competent formation of his lifestyle. Healthy, sound sleep, walking, quitting smoking and drinking alcohol. A person with heart pain should rest more and spend less time on the computer and TV.
Sports activities are useful, namely swimming, aqua aerobics, running, Nordic walking, fitness, yoga. A big plus for VSD is skiing or cycling. A contrast shower after training is useful. It is important to avoid sudden movements and jumps while playing sports.
Myths and reality
There is an opinion that a rapidly beating heart wears out faster, and therefore bradycardia with VSD is a kind of luck.
But it’s worth dispelling this myth. Firstly, a low heart rate is the norm only for a trained heart, the owners of which are mainly athletes. 40-50 beats per minute is the absolute norm for such people, and their bodies do not feel anything pathological. Secondly, poor cardiac output is fraught with hypoxia of organs, in particular the brain. This can lead to convulsions, loss of consciousness, cardiac arrest - if the bradycardia is pronounced and is not treated for a long time. You should not think that a slow pulse can stop the heart at any time. Dystonics very often pay increased attention to their cardiomuscle, constantly counting its contractions. Therefore, often with VSD, cardioneurosis develops, which in turn leads to depression. In addition, you should not be afraid of a low heart rate at night, this is a natural process. There are patients whose heart rate at night is up to 35 beats, and this does not lead to death - provided that the heart is healthy.
A low pulse with VSD usually does not threaten any complications, since it is associated not with organic diseases, but with vegetation. But sometimes, due to the individual perception of the patient, it is accompanied by the following symptoms:
- headaches of various types;
- decrease in blood pressure and temperature;
- motion sickness (in transport);
- feeling unwell and stuffy;
- confusion of thoughts;
- feeling of impending fainting;
- unpleasant sensations in the chest (squeezing, bloating, discomfort, tingling);
- loss of normal coordination;
- increased sweating due to nervousness;
- pale or bluish skin;
- fear of death, increased anxiety;
- drowsiness, lack of concentration, absent-mindedness.
VSD sufferers experience exacerbation of bradycardia (as well as other types of arrhythmias) more often during the demi-season periods of the year. In regions with an unstable climate and cold summers, it is much more difficult for patients. Any change in weather can affect your heart rate.
Are panic and anxiety conditions really dangerous for the heart?
On the one hand, the heart is an organ that is involved in all significant processes occurring in the body. The consequences of a neurotic disorder for the heart and cardiac muscle cannot be underestimated. Psychiatrists and neurologists note that progressive neurosis negatively affects the patient’s heart, head and stomach, contributing to the development of psychosomatic diseases affecting these organs. The heart also responds to a person’s fear and anxiety, regardless of whether they are justified or groundless.
Panic states most often begin with vague anxiety, and already then the first heart rhythm disturbances occur. As fear and anxiety increase, disruptions intensify. This activates a mechanism that informs all systems and subsystems of the body about a problem that has arisen. The blood flow increases, the so-called emergency system is mobilized. A panicked person, like an astronaut before going into outer space, is prepared by caring organ assistants for action in extreme conditions. And the heart, like a special unit after an emergency is declared, begins to work at an increased rhythm.
However, no response is made by a mobilized, carefully prepared person. Instead of engaging in a fight with the enemy (who is absent), he shows complete passivity: he hides in a corner, goes to bed, or rushes aimlessly, not understanding what is happening to him, but only strengthening his painful state with this unconstructive inaction.
Law enforcement officers who have worked for a certain period in an intensive regime are given rest to recover. A similar recovery period is also needed for the heart, the brain, the stomach, the circulatory system... and the patient himself who has experienced panic. However, no one gives him, as a hero, additional vacation or even a day off. After an attack of panic, normal life returns to normal, and the victim of panic attacks returns to his family or work, where no one takes into account the fact that he “worked a shift in heavy duty.” On the contrary, if his problems are already known to others, everyone considers him almost a parasite. After all, the cardiologist, to whom the patient turned with complaints of heart ailments, probably also pronounced a verdict that he was healthy. What other conclusion could the doctor make if neither the cardiogram, nor the 24-hour monitor, nor the test results showed any abnormalities?
Main signs and symptoms of cardiac bradycardia
Bradycardia is a condition when the heart rate (HR) decreases, that is, a person's heart beats very slowly. The disease does not develop independently, but is a symptom of both cardiac pathology and diseases of other organs. In people with signs of bradycardia, the pumping function of the heart is impaired, which leads to stagnation of blood in the respiratory organs. Due to these symptoms, a lung abscess may develop. But sometimes bradycardia is a physiological norm, being a feature of people with a healthy heart or trained athletes.
The main reasons for the development of bradycardia symptoms in humans are divided into forms:
- Extracardiac, which develops with neuroses, vegetative-vascular dystonia, high blood pressure, pathologies of the brain, gastrointestinal tract, endocrine.
- Organic, developing against the background of cardiosclerosis, myocardial dystrophy, myocardial infarction.
- Drug-induced, occurring during treatment with drugs such as quinine, cardiac glycosides, sympatholytics, morphine, calcium channel blockers.
- Toxic, which occurs with an extreme degree of intoxication of the body during hepatitis, infectious diseases, uremia, phosphate poisoning.
- Physiological, developing against the background of regular smoking, unprofessional chest massage, and constant cold.
- Senile, which is the cause of natural aging of the body.
Severe bradycardia causes disruptions in the functioning of all body systems. During symptoms, circulatory disturbance occurs, which is directly related to oxygen starvation, which causes a person to lack the strength for normal life activities. Bradycardia is often accompanied by pallor of the mucous membranes and skin, convulsions and even loss of consciousness. The main symptoms of the disease that require immediate treatment include:
- chronic fatigue, weakness;
- lack of air, difficulty breathing;
- frequent dizziness;
- disturbance of attention, memory;
- increased or decreased blood pressure;
- short-term visual disturbances.
Characteristics of psychogenic disorders
The occurrence of extrasystole during panic attacks occurs mainly against the background of psychogenic disorders that disrupt the heart rhythm. Please note that heart problems can also occur when the structure of the heart muscle changes. The emerging feeling of fear only increases the heartbeat and causes the development of disorders such as arrhythmia.
The attack cannot be relieved even with the help of antiarrhythmic medications. In order to help a person, you need to provide complete safety conditions for him - call an ambulance or take him to the hospital. Even at home, the condition can quickly return to normal without the use of any medications.
If the patient was in a hospital under 24-hour medical supervision, then after discharge from the medical institution, attacks often recur. When a person is left alone with himself, he can succumb to his own fears. When such attacks occur, doctors identify arrhythmia that develops against the background of disorders such as psychogenic disorders. The reason for this is disturbing thoughts that appear regardless of the patient’s wishes.
Be prepared for a comprehensive examination in the hospital
Diagnosis of the disease
The therapist diagnoses bradycardia, paying attention to the patient’s complaints, his heart sounds, rare pulse, and respiratory arrhythmia. If there are symptoms of heart failure, the patient will be referred for examination and treatment to a cardiologist. Basic methods for diagnosing bradycardia:
- Electrocardiogram. With its help, doctors record a decrease in heart rate, the presence of sinoatrial or atrioventricular block. With prolonged symptoms of bradycardia or with unsuccessful treatment, daily ECG monitoring is required.
- CHPEFI. If the ECG method does not detect blockades, then a transesophageal electrophysiological study is prescribed, in which the cardiac conduction pathways are examined, revealing organic or functional bradycardia.
- Exercise bicycle ergometry, which evaluates the heart rate during a certain physical activity.
- Ultrasound of the heart, if an organic form of bradycardia is determined. Ultrasound examination will determine sclerotic and degenerative changes in the myocardium, an increase in the size of the heart.
How to learn to control your consciousness?
To begin treatment, become the master of your consciousness. To do this you need:
- Know clearly what you want. Determine your goal and go towards it. Don't notice failures and falls. Then you will have a clear step in life and a confident heart rate.
- Play sports not for results, but for health. Give your body moderate physical activity regularly. During training, the heart will receive confident signals that are not afraid of negative impulses.
- Get acquainted with yoga or auto-training.
Agree that this is not difficult to do! Just a wish is enough!
Continue further treatment by reading our recommendations on the website on how to get rid of VSD.
We recommend watching:
We recommend reading:
VSD and pregnancy
Previous article
Respiratory exercise for VSD
Next article
First aid for an attack of bradycardia
If you feel the main symptoms of bradycardia (dizziness, weakness), doctors recommend taking the following measures:
- brew strong coffee;
- do any physical exercise or go for a run;
- use Zelenin drops for bradycardia to quickly increase your heart rate.
If the tonometer shows a heart rate below 35 beats/minute, call an ambulance, lie on your back with a small cushion under your head, and place your legs on pillows. When pain in the heart area is observed with symptoms of bradycardia, it is advisable to place a nitroglycerin tablet under the tongue. If the patient has lost consciousness, the emergency measures are as follows:
- Artificial respiration. Pinch the victim's nose with one hand and place the other under the neck. Take a deep breath, press your lips tightly to the victim’s lips, and exhale into the patient’s mouth. If everything is done correctly, the person will exhale air on his own. Measure the patient's pulse after three injections, continuing manipulations until the victim's ability to breathe on his own is restored.
- Indirect cardiac massage. If the patient's pulse cannot be felt, then pressure should be applied to his chest in the area of the heart. This will help restore breathing and restore blood circulation. Place one palm perpendicular to the victim's neck on the third lower lobe of the chest, and the second on top. Apply 10-12 quick, short pressures, then perform two artificial respirations. Provide assistance until the patient’s breathing is restored or until an ambulance arrives.
Heart and panic attacks
Panic attacks, which in modern medicine are inextricably linked with vegetative-vascular dystonia, entail, in addition to fear and anxiety, a number of unpleasant, painful physical symptoms.
Patients who have experienced panic attacks named the following among the most striking manifestations accompanying panic:
- Frequent pulse, tachycardia.
- Erratic pulse, extrasystole and arrhythmia.
- Pressure and pain in the chest area.
These symptoms are unpleasant not only because of their sensations. Any ailment related to the heart causes fear. After all, the heart is our leading working organ, a tireless pump on which the body’s blood supply, and therefore life, depends. Any cardiac pathology can cause serious illness, disability and even death.
Surgical treatment of the disease
Complete recovery from the symptoms of bradycardia is possible with the help of surgery. This is due to the implantation of a pacemaker, which controls the functioning of the heart muscle. A stimulator is a microcomputer equipped with an electrical pulse generator and electrodes, thanks to which the patient does not experience any symptoms of bradycardia. The pacemaker program is selected individually, in which the frequency of heart contractions, impulse strength and other heart parameters necessary for the normal functioning of the body are regulated.
Treatment of bradycardia with a pacemaker is prescribed in the following cases:
- The patient has regular fainting spells.
- Bradycardia is combined with tachycardia, which makes it impossible to use a number of medications for treatment.
- Progression or chronic form of heart failure.
- Drug treatment was not fruitful.
- Symptoms of bradycardia developed while taking medications that cannot be excluded for an additional disease.
The operation to insert a pacemaker is performed under general anesthesia and lasts about an hour. The stimulator is injected into the right atrium through the veins. To do this, the cardiac surgeon makes an incision in the area of the collarbone, abdominal cavity or fat layer, monitoring all manipulations using an X-ray machine. After such surgical treatment, the patient lies in the intensive care ward on his back for two hours, after which he is transferred to a regular ward. Complete recovery from bradycardia symptoms occurs after two months. Your pacemaker should be replaced every five years.
Medications
In the early stages of the disease, successful treatment is carried out with the following medications:
- "Atropine sulfate". Instantly relieves an attack of bradycardia by blocking inhibitory receptors and activating stimulating ones. The drug is administered intravenously, 1 ml of a 0.1% solution. Care must be taken in dosage, because even a slight overdose causes side symptoms: dilated pupils, impaired visual perception, dry mouth, tachycardia, loss of intestinal tone, difficulty urinating, dizziness.
- "Izadrin." Has a stimulating effect on beta-adrenergic receptors. This is the best drug that quickly eliminates an attack of bradycardia when it is associated with the contractile function of the heart muscle and increased excitability. It is used for loss of consciousness and some forms of cardiogenic shock. The drug is administered intravenously by drip along with a glucose solution at a dose of 0.5-5 mcg/minute.
- "Ipratropium bromide." Causes a prolonged and pronounced increase in heart rate with symptoms of bradycardia. Reduces the secretion of glands, dilates the bronchi. Does not affect the nervous system. The oral dose for symptoms of bradycardia is 1 tablet 3 times a day. Treatment with the drug is contraindicated for glaucoma, tachycardia, enlarged prostate gland, and in the first trimester of pregnancy.
- "Ephedrine hydrochloride." In its action, the drug is close to adrenaline, causing, with severe symptoms of bradycardia, vasoconstriction, dilation of the bronchi, inhibition of intestinal motility, increased blood pressure, which leads to excitation of the conduction system of the heart. The medicine is available in tablets and ampoules. Treatment is prescribed in a dose of 30-50 mg, and it must be taken every 4 hours. You should not drink Ephedrine before bed to avoid insomnia. Treatment with the drug is contraindicated for diseases of the thyroid gland, atherosclerosis, and organic heart disease.
- "Apressin." A blood pressure medicine for symptoms of bradycardia, relieving spasms of small arteries, reducing blood pressure, increasing heart contractions. "Apressin" improves cerebral and renal blood flow, cerebral vascular tone, and has a moderate sympatholytic and adrenolytic effect. The drug is prescribed for symptoms of bradycardia in the amount of 1 tablet 2-4 times a day after meals with a gradual increase in dose. The doctor prescribes the course of treatment individually from 2 weeks to 1 month, with a dose reduction towards the end of therapy.
Common causes of heart failure due to blockades and arrhythmias
cardiac cycle, the functioning of the cardiac conduction system is normal
The reasons for interruptions during blockades and arrhythmias lie in changes in the basic functional abilities of the main organ:
- Automaticity;
- Excitability;
- Conductivity;
- A combination of these disorders;
Changes can be both organic and functional in nature, formed under the influence of various disorders:
- Vegetative;
- Endocrine;
- Electrolyte;
- Metabolic reactions in the heart muscle;
- Congenital features of the conduction system of the heart.
Meanwhile, blockades and arrhythmias have their own reasons, which at the same time are the causes of interruptions in heart rhythm. Of course, often the heart beats intermittently due to formed or congenital cardiac pathology; it requires treatment, but treatment not of the interruptions themselves, but of the conditions that caused them, that is, in each specific case it is necessary to treat the disease, not the symptom.
All these issues will be addressed in the relevant sections of this article, except for flutter and ventricular fibrillation. Although there is undoubtedly an interruption in the heart, in this case a person can hardly complain about the feeling of interruptions. His condition will not allow this. Ventricular fibrillation and flutter is a terminal cardiac disorder that develops against the background of severe heart pathology (drug intoxication - cardiac glycosides, sympathomimetics, acid-base imbalance, electric shock, extensive myocardial infarction, hemotamponade, etc.) - usually a person quickly loses consciousness and simply does not have time to explain anything, he has no pulse, he dies.
Folk remedies for the treatment of cardiac bradycardia
Alternative medicine can be very effective at the first symptoms and for the prevention of bradycardia. Folk remedies are aimed at stimulating the heart muscle. The most accessible:
- Lemons, honey, garlic. Take 10 medium-sized fruits, scald with boiling water, squeeze out the juice. Chop 10 cloves of garlic and add to lemon juice. Pour 1 liter of honey into the resulting mixture, and then keep in a cool, dark place for 10 days. To eliminate the symptoms of bradycardia, take the drug daily for 3 months, two tablespoons in the morning on an empty stomach. To consolidate the results, repeat the course of treatment every year.
- Vodka, propolis tincture, garlic. Grind 100 g of garlic, add to it 25 ml of propolis tincture (pharmacy), 250 g of vodka, leave for 10 days in a dark place. Take the remedy for the treatment of bradycardia before meals 3 times a day, 1 teaspoon, until the symptoms of the disease subside.
- Rose hip. The fruits are useful for strengthening the heart when symptoms of bradycardia are detected. Take 8-10 rose hips, add 400 ml of water, boil for 15 minutes. Cool the broth, strain, add 3 tablespoons of May honey, stir. Take 50 ml daily 30 minutes before meals 3 times a day until the symptoms of bradycardia completely disappear.
During the treatment of bradycardia and to prevent its symptoms, it is advisable to introduce flaxseed or olive oil, fish oil, seaweed, and pollen into the daily diet. These products help strengthen the heart muscle and eliminate symptoms of the disease such as dizziness, increased fatigue, and darkening of the eyes. Watch the video for some more useful folk recipes for treating bradycardia at home:
Paroxysmal tachycardia
Interruptions of heart rhythm during paroxysmal tachycardia (atrial, ventricular, atrioventricular) occur suddenly. For no apparent reason, the patient feels a push in the chest, followed by frequent heartbeats (from 140 to 240 beats/min). The symptoms of paroxysmal tachycardia are similar to those of extrasystole. In addition to rhythm disturbances, this pathology is characterized by other symptoms reminiscent of autonomic dysfunction:
- Dizziness;
- Muscle tremors;
- Sweating;
- Frequent urge to urinate with the release of considerable volumes of urine;
- Excitation;
- Anxiety states.
variants of paroxysmal acceleration of the heart rate (paroxysmal tachycardia)
In the case of organic damage to the heart muscle, there is a risk of developing heart failure.
Interruptions in the heart during paroxysmal tachycardia consist in the fact that first the patient hears a jolt, and then frequent beats, but interruptions in the pulse are not typical for this pathology. Frequent, small-filled pulse - rhythmic, no missed beats.
Treatment of paroxysmal tachycardia, if possible, is carried out in a hospital setting, where it is easier to control. Upon discharge home, the patient receives recommendations regarding further treatment and prevention of attacks.