1
Author of the article: Marina Dmitrievna
2018.09.15
127
Treatment
All older people know the song performed by Leonid Utesov with the words “Heart, you don’t want peace!” And although the author of the text did not at all put a physiological meaning into these words, the heart really, even if it wanted to, cannot allow itself peace. 10-20 seconds after the heart stops, a person loses consciousness. If the heart fails to start within five to six minutes, the person dies.
The heart, like all other organs, is susceptible to diseases that adversely affect its functioning. Man has invented many medications to treat heart diseases. But there are diseases when medications cannot help. The heart or its affected parts need to be replaced.
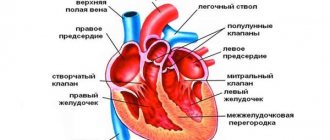
Heart and its vessels
The history of the discovery of the mechanical heart
The pioneer of the possibility of maintaining blood flow through vessels outside the body was the Soviet doctor Demikhov. He performed an operation on a dog back in 1937, installing a pump in place of the heart, which was connected to an electric motor. In the 60s, American scientists Kolf and Akutsu created a heart made of plastic with 4 tricuspid valves. Its operation was ensured by a pneumatic drive.
But the real successful implantation of an artificial heart was carried out only in 1969 by a surgeon from America Cooley. The patient suffered from a left ventricular aneurysm. He underwent extensive resection (removal) of part of the myocardium, after which it was impossible to disconnect him from the extracorporeal circulation machine.
Since the only chance to save a life would be a heart transplant, a mechanical transplant was installed before it was performed. He worked for 64 hours, then a donor heart was found and transplanted. Unfortunately, the patient died of pneumonia, having lived less than 2 days. But such two-stage transplantation is the basis of modern operations.
All further attempts to create an artificial analogue of the heart did not lead to the expected result. Models of Russian devices can work up to 100 days, their external engine is bulky, and must be recharged every 12 hours.
The first such device was connected to a patient at the Bakulev Center in 2010. It can be used for now as a temporary rescue for patients awaiting a heart transplant.
Since the demand for artificial hearts increases every year, devices and scientific discoveries in this area are constantly being improved. The newest, but experimental developments include a 3D printed heart, as well as one grown from stem cells.
We recommend reading the article about installing a pacemaker. From it you will learn about the purpose of installing the device and its types, implantation methods and possible complications.
And here is more information about myocardial hypertrophy.
Artificial heart
An artificial heart or artificial ventricles are used in patients with end-stage heart failure to save their lives and maintain circulation until a suitable donor organ is found for heart transplantation. In some patients with contraindications for heart transplantation (age, concomitant diseases, etc.), an artificial heart (in our Center we use systems such as HeartWare, or HeartMate 3) can be implanted as a final option.
Our Center carries out the world's largest program for the implantation of long-term artificial circulatory support systems. In our Center, more than 1,000 patients have been observed or are still being observed for more than a year after implantation of an artificial heart, and more than 300 patients for more than three years and more than 100 patients for more than five years. These patients are with their family or working in their previous profession. In rare cases, especially after surgery on a weakened heart or in acute massive myocardial infarction, short-term mechanical support of a weakened heart using the Impella system is used for several days.
The Center regularly trains doctors from various clinics in Europe and America. We provide certified advanced training and training in the use of new systems for surgeons, cardiologists and perfusionists at centers starting artificial ventricular implantation programs. The international congress, which our clinic organizes once every two years, is one of the largest and most attended congresses on this topic in the world. The Center operates a European data bank on the use of long-term mechanical circulatory support.
In total, from the founding of the Center to May 1, 2020, various types of artificial hearts were used in 2,715 patients. In 481 patients, a heart transplant was subsequently successfully performed; in 263 patients, the artificial heart was removed after their own heart regained its function. In patients with contraindications for heart transplantation (mostly patients over 65 years of age), an artificial ventricle is implanted as definitive therapy. Currently, more than 40% of our patients on an artificial ventricle are over 60 years of age (see Fig. 20). Thus, an artificial heart, along with a donor heart transplant, is one of the most effective methods of treating patients with end-stage heart failure at any age. In our clinic, as of May 1, 2020, more than 500 patients had an artificial heart implanted on a permanent basis. Currently, almost 400 patients are being observed after implantation of artificial ventricles of various types in our Center: some of them have already been discharged home, others are awaiting discharge. Some patients were so satisfied with the results of the operation and the improvement in their quality of life that they refused further heart transplantation.
You can watch a film that demonstrates the implantation of an artificial left ventricle of the heart such as HeartWare HVAD. The operation is performed by the leading cardiac surgeons of the clinic, Evgeniy Potapov and Thomas Krabach. The operation is performed through a minimally invasive approach without opening the sternum and without the use of a heart-lung machine (ACB). The operation lasts less than 2.5 hours, the patient is discharged home after 10 days. The technique shown was developed and introduced into clinical practice by the leading cardiac surgeon of the clinic, Evgeniy Potapov, and is a standard operation in Berlin.
One of the patients with an artificial left ventricle trains on roller skates. He set himself the goal of running a marathon on roller skates. In September 2014, the patient gave an extensive interview to one of the German television channels. You can watch this interview (in German) here. In 2017, the patient underwent a successful heart transplant.
The average age of our artificial heart patients is just under 55 years, more than 500 patients were over 70 years of age and three were over 80 years of age at the time of artificial heart implantation (see Fig. 15b).
A special place is occupied by the use of artificial hearts in children. Our Center has developed and successfully implants the BerlinHeart system into patients. This system can be used in newborns weighing from 2000 grams. More than 180 children received an artificial heart in our Center. Based on our experience, the pediatric Berlin Heart Excor artificial heart and the methodology for its use, developed by us, are successfully used all over the world. More than 1,500 surgeries were performed in the United States and
Canada, there is experience of use in Europe and Asia. The only child who received an artificial heart developed by us at the Bakulev Institute in Moscow was successfully transplanted with a donor heart in Italy.
The table below shows the types of artificial hearts used in our Center since 1986
| Rice. 1. Model 1986 BerlinHeart artificial heart | Rice. 2. The first operation to implant an artificial heart was performed in 1987. | Rice. 3. Artificial ventricles BerlinHeartt Excor |
In Fig. Figure 1 shows a model of an artificial heart developed in Berlin. This model was first implanted by Professor Hetzer in 1987 (Fig. 2). A total of two successful operations were carried out. After this successful experience, the Center switched to the implantation of artificial ventricles from BerlinHeart, shown in Fig. 3.
| Rice. 4. Scheme of operation of the artificial ventricle | Rice. 5. Artificial ventricle |
In 1998, for the first time in the world, an artificial ventricle was implanted with a fundamentally new operating principle, designed with the participation of NASA specialists and Michael DeBakey. This small pump weighing only 93 grams is capable of pumping up to 6 - 7 liters of blood per minute and thereby ensuring the normal functioning of the entire body (Fig. 4 and 5).
In 2002, a miniature artificial ventricle INCOR with magnetic supports was also implanted for the first time in our Center.
| Rice. 6. Left-sided artificial ventricle INCOR with control unit | Rice. 7. Left-sided artificial ventricle INCOR | Rice. 8. Prof. Hetzer with the first two patients a few days after the operation |
In Fig. 6, the left-sided artificial ventricle INCOR is shown together with the control unit and two batteries located outside. In Fig. 7 this system is presented separately. It is capable of pumping up to 10 liters of blood per minute with a power consumption of about 4 - 5 W.
Thanks to the magnetic turbine support, there is no friction or wear of parts.
| Rice. 9. Three-dimensional reconstruction of computed tomography. The inlet cannula is sutured to the apex of the heart, and the outlet cannula is sutured to the descending part of the thoracic aorta. | Rice. 10. INCOR is indicated at the time of surgery |
| Rice. 11. A patient undergoing implantation of a MicroMed DeBakey artificial left ventricle at his former job as the owner of a cleaning company. A small bag with batteries and a control unit is clearly visible on the left side | Rice. 12. Dr. E. Potapov and a patient with an artificial left ventricle (type HeartMate II) during a seminar on training commanders of special forces of the Berlin police. Annual seminars introduce the leadership of the Berlin police to the characteristics of patients on artificial circulatory support. |
| Rice . 13. Diagram of implantation of two HeartWare pumps as biventricular support | a) Front view | b) Side view |
| Rice. 14 . X-ray of a patient with biventricular support such as HeartWare | ||
Rice. 15 a
Rice. 15 b
The latest model of the artificial ventricle HeartMate 3 (Fig. 15 a), in the development and testing of which the leading cardiac surgeons of our clinic, Dr. E. Potapov and Dr. T. Krabach, took part. The pump is indicated during surgery immediately after implantation into the apex of the left ventricle.
This pump can also be used as biventricular circulatory support. This option as computed tomography is shown in Fig. 15 b.
1 – HeartMate 3 pump implanted in the right atrium to support the pulmonary circulation
2 – prosthesis that goes around the root of the lung and is connected to the pulmonary artery
3 – anastomosis with an additional prosthesis of smaller diameter
4 – HeartMate 3 pump, implanted in a standard technique into the apex of the left ventricle to support systemic circulation
| Rice . 16a . Patient after implantation of HeartWare type BVAD. The patient holds a bag with a control unit in one hand. The other bag is held by Dr. Evgeniy Potapov | Rice . 16b . On the left is an 82-year-old patient with left-sided support (HeartWare type), in the middle is an 81-year-old woman with left-sided support (Jarvik 2000 type) and on the right is a 77-year-old patient with Heartassist5 |
Rice. 17 Our patients during sports, at home and at leisure
Currently, more than 300 patients are on artificial circulatory support, many of them for more than two years. The lifespan of an artificial heart is not limited; some patients live for more than 8 years. The vast majority of patients with an artificial heart are at home and lead an active lifestyle.
Rice. 18. Currently, more than 300 patients are on artificial circulatory support, many of them for more than 5 years.
About 20% of patients with dilated cardiomyopathy who are placed on a ventricular assist tend to improve their heart function. About half of them recover their heart function so well and long-term that they no longer need an artificial heart. In our Center, in more than 100 patients in similar cases, the artificial ventricle was removed, and the good function of their own heart remained for years. To simplify the removal of an artificial heart ventricle, our Center has developed a special technique. We use special titanium plugs that we have developed. After removing the artificial ventricle and closing the defect with a titanium plug, its surface is completely covered with connective tissue within 6 months. You can read the details in the article published in the Journal of Heart and Lung Transplantation. A similar operation was successfully performed on a patient from Russia. After almost a year on mechanical circulatory support, the patient’s own heart recovered, and the artificial heart was removed using a titanium plug developed in our Center.
Recently, in our Center, a technique for implanting a left-sided pump as a biventricular support was developed and successfully used in more than 50 patients. In patients with biventricular failure, we implant, after certain modifications, two pumps of the HeartWare or HeartWare 3 type inside the pericardium (Fig. 15a). If previously patients had to pull carts with a compressor weighing 20 kg, and they had 2 artificial ventricles on their stomachs outside the body, now such patients wear two bags over their shoulders (both 2.5 kg each), connected by a thin cable with pumps inside chest. The implantation scheme is shown in Fig. 13 and 14, 15a, and the patient after surgery in Fig. 16a. You can read more detailed information in the article by Dr. Potapov.
| Rice. 19. Title page of the “Journal of Heart and Lung Transplantation” with photographs of the operation to remove the artificial ventricle and implantation of the plug, carried out in our Center after restoration of the native function of the left ventricle. Such operations are carried out under the guidance of the director of the clinic, Prof. Hetzer senior doctors of the clinic Dr. Krabatch and Potapov | |
| Rice. 20 a | Rice. 20 b |
| Rice. 20. X-ray images of the patient before and after removal of the artificial ventricle of the heart. The first picture (a) shows the HeartMate II artificial heart, the second (b) shows a titanium plug developed in our Center | |
Rice. 21. Development of a program of mechanical circulatory support in our center. The number of implantation systems is constantly increasing. Three quarters of these are fully implantable systems for long-term circulatory support.
Rice. 22 . More than 40% of our patients on artificial ventricle are over 60 years of age
Rice. 23. Privatdozent E. Potapov and his patient Oleg Malkhov, Chairman of the All-German Union of Police Workers
Different types of artificial heart used at the German Heart Center in Berlin as of May 1, 2018.
| Type of artificial heart | Duration of use | Configuration | Blood flow type | Position | Number systems |
| Bucherl Heart | Long-term | TAH | Throbbing | Inside the body | 2 |
| Berlin Heart* | Long-term | BVAD/RVAD/LVAD | Throbbing | Next to the body | 786 |
| Novacor LVAS | Long-term | LVAD | Throbbing | Inside the body | 116 |
| TCI (HeartMate) | Long-term | LVAD | Throbbing | Inside the body | 23 |
| Combination* | Long-term | BVAD | Both | Both | 325 |
| MicroMed* DeBakey | Long-term | LVAD | Constant | Inside the body | 47 |
| Abiomed BVS 5000 | A short | BVAD/RVAD/LVAD | Throbbing | Next to the body | 47 |
| Hemopump | A short | LVAD | Constant | Next to the body | 32 |
| Biomedicus | A short | BVAD/RVAD/LVAD | Constant | Next to the body | 26 |
| Arrow LionHeart | Long-term | LVAD | Throbbing | Inside the body | 6 |
| Impella* | A short | BVAD/RVAD/LVAD | Constant | Inside the body | 117 |
| Incor* | Long-term | LVAD | Constant | Inside the body | 214 |
| CardioWest TAN* | Long-term | TAH | Throbbing | Inside the body | 53 |
| DuraHeart | Long-term | LVAD | Constant | Inside the body | 18 |
| CorAid | Long-term | LVAD | Constant | Inside the body | 1 |
| HeartMate II* | Long-term | LVAD | Constant | Inside the body | 244 |
| HeartMate III* | Long-term | LVAD | Constant | Inside the body | 153 |
| Levitronix* | A short | BVAD/RVAD/LVAD | Constant | Next to the body | 434 |
| Jarvik 2000 | Long-term | LVAD | Constant | Inside the body | 13 |
| Ventrassist | Long-term | LVAD | Constant | Inside the body | 4 |
| HeartWareHVAD* | Long-term | BVAD/RVAD/LVAD | Constant | Inside the body | 953 |
| C-Puls* | Long-term | LVAD | Constant | Inside the body | 6 |
| Circulite | Long-term | LVAD | Constant | Inside the body | 1 |
| Total: | 33307 | ||||
| * – systems currently used | |||||
November 6, 2005 At the Russian Research Center for Surgery of the Russian Academy of Medical Sciences, a unique cardiac surgery “implantation of artificial heart ventricles” (Implantation of the BVAD) was performed on a patient with terminal stage cardiomyopathy.
You can also read the following reports on this topic.
“New parameters for determining an individual treatment strategy for patients with terminal heart failure”, private associate professor Dr. med. cardiac surgeon Evgeniy Potapov .
“Stem cells and mechanical circulatory support” by Dr. Boris Nasseri, read in November 2006 at the congress dedicated to the 20th anniversary of the German Heart Center in Berlin.
“ Mechanical circulatory support.” A project within the framework of cooperation between DHZB and VSMA named after. N. N. Burdenko
Prevention and treatment of percutaneous cable infection in patients with long-term mechanical circulatory support. E. Potapov, R. Hetzer and the working group on heart transplantation and MPC of the German Cardiological Center in Berlin.
“ Treatment of patients in the terminal stage of chronic heart failure using mechanical circulatory support . The lecture was given by Dr. Potapov on December 6 at a meeting of the Russian Society of Cardiovascular Failure.
The German Heart Center in Berlin, together with the Academy of Life Sciences, offers an internship at the German Heart Center in Berlin on the topic “Mechanical circulatory support and heart replacement”.
You will receive more detailed information on the Academy page. The internship is intended for doctors and perfusionists, regardless of the country of residence, and is designed for 2 years of work at the Center. The scholarship is 2500 euros per month. Please send inquiries in English or German to https://www.lifesciences.net/programs/mcshr.html
You can read the report given by Priv.-Assoc., Dr. med. Potapov E. in Moscow 30.03. 2020
“Surgical treatment of heart failure”
Rice. 25. Cover of the report
Successful examples of installing an artificial organ in different countries
For a long time, the most famous mechanical heart was the Jarvik 7 model, the record life expectancy of the patient was 620 days. This is how long W. Schroeder has lived since its installation (in 1985), proving that it is possible to replace a biological organ with a man-made one.
Jarvik 7 artificial heart model
The next version of such a device was Symbion, and at present Syncardia is practically the only successful model of artificial hearts. The main problem with such devices is the weight of the charger, which had to be carried with you or carried in a backpack behind your back.
Patients with such a device are not spared the need for a donor organ transplant, but they can expect a transplant not only in the hospital, as was before, but can charge the battery from a regular outlet while at home. Syncardias were installed in 1,600 patients; the maximum duration of work exceeded 3.5 years. Therefore, patients have a chance to live until a suitable donor is found.
Artificial heart on the right
If life is precious...
The AbioCor heart now costs just under 100 thousand dollars, the VentrAssist will cost about 50. However, this price is significantly less than the costs associated with each donor heart transplant.
If we also take into account the funds spent on medical care for patients with heart failure, it becomes clear: an artificial heart is not only useful, but also beneficial for the medical industry. And financial incentives, as you know, are the strongest. Including for technical progress.
It only remains to clarify that supporting this progress at the cost of one’s own life is completely optional. With timely prevention of heart disease, your own heart can last much longer than 50 years. And most importantly, practically free.
What is heart transplant syndrome?
Despite the chance of life after a mechanical heart transplant or replacement of its valves, many patients do not feel relief. This is due to the following reasons:
- there is a fear of device failure,
- noise from work at night makes it difficult to sleep,
- the patient is constantly fixed on the rhythm of the heartbeat,
- Depression and suicidal tendencies increase.
There are complaints of headache, numbness of the extremities, fainting and dizziness, severe fatigue. This forces patients to sharply limit physical activity.
One of the concerns is the lack of pain when the device malfunctions, so patients are afraid of losing control over their health. Such symptoms are treated jointly by a cardiologist and a psychiatrist.
Risks of installing the device
The operation is quite complex, it has predictable and sudden complications. For example, no doctor can guarantee that death will not occur during the installation of a mechanical heart.
Fairly expected risks include:
- allergic reactions to medications,
- formation of blood clots,
- intense bleeding
- infection,
- breakdowns or interference in the operation of the mechanism.
Still, most operations are successful and without complications, and patients with an artificial heart are even able to run a marathon. It all depends both on the disease and on the patient’s desire for recovery and compliance with the doctor’s recommendations.
Watch the video about installing an artificial heart:
Wireless heart
Now that we have assessed the scale of the task, let's see how it is solved in relation to the heart. Denver-based Abiomed's AbioCor is a real artificial heart that replaces both ventricles and supplies blood to the lungs and other organs. The device, the size of a grapefruit and weighing 900 grams, contains a titanium pump, control unit and battery. Its capacity is enough for 30 minutes of battery life, and charging occurs through the skin: that is, no wires come to the surface of the body. An external battery worn on the belt allows you to remain without recharging for several hours.
This device is intended for patients with end-stage heart failure and poor prognosis. Moreover, the creators of the device claim that it allows patients not only to “live”, but guarantees them a completely acceptable quality of life.
The first AbioCor heart was transplanted in 2001. Since then, no more than 20 devices have been installed, but the company is optimistic about the device’s prospects and estimates the market at 100,000 operations per year.
Cardiopulmonary bypass systems
Extracorporeal circulation, that is, connecting the patient’s vascular network to devices for cleaning, oxygenation or administration of medications, can be of the following types:
- general,
- isolated,
- auxiliary.
A common option involves using a mechanical pump and oxygenator instead of the heart and lungs. Such heart-lung machines are widely used in cardiac surgery.
If it is necessary to isolate an organ or system from the general bloodstream in order to maintain a large concentration of a medicinal substance, then this method is called regional or isolated. It is used by oncologists and surgeons for the perfusion of cytostatics or antibiotics.
Circulatory support reduces cardiac workload by reducing blood flow or peripheral vascular resistance. It is carried out in the form of intra-arterial balloon counterpulsation, unloading when connected to roller or centrifuge pumps, as well as installation of artificial heart ventricles.
History of artificial perfusion devices
These devices are designed to keep a person alive when the heart is completely or partially unable to perform its functions.
The first attempt to create an AIC was made at the end of the nineteenth century, when German scientists Frey and Gruber invented the first mechanical device for artificially pumping blood and enriching it with oxygen. In the Soviet Union, the first development of AIC dates back to 1926. The apparatus (autojector) was created by two scientists Bryukhonenko and Chechulin. The device worked well in experiments on dogs, but the autojector did not find use in clinical medicine.
The creation of AIC in the world continued, and the first significant use of the device occurred in 1952. Cardiac surgeon Dodrill in the United States performed successful open-heart surgery using an AIC. Moreover, Dodrill used a device that he developed himself in collaboration with General Motors.
Five years later, heart surgery was performed in the USSR.
What is a heart-lung machine?
The device, which can take over the basic functions of the body - breathing and blood circulation to transfer oxygen to tissues, includes the following parts:
- oxygenator (analogue of lungs),
- heat exchanger (maintains temperature),
- pump with capacity regulation (artificial heart),
- blood circulation lines,
- filters for absorbing gas bubbles, blood clots, destroyed blood cells.
Additionally, it may include systems for absorbing blood from the wound area, draining the left ventricle, measuring blood flow speed, venous and arterial blood temperature, pressure, and oxygen content. To refill the device the following can be used:
- physiological solution of glucose or sodium chloride,
- rheopolyglucin,
- potassium chloride,
- bicarbonate of soda,
- red blood cells from donor blood.
Work principles
Connecting a machine for artificial blood circulation depends on the chosen surgical procedure. The most common scheme involves the following steps:
- Blood sampling from both vena cava or from the right atrium, ventricle.
- Entering the oxygenator.
- Pumping into the femoral artery.
- Advancement along the abdominal and thoracic part of the aorta (against the usual direction).
- Through the aortic arch, blood flows into the coronary and cerebral arteries.
The duration of the connection depends on the type of operation - from several minutes to 4 - 8 hours. In this case, the doctor tries to keep the patient on artificial perfusion as little as possible. If the operation requires more than an hour, the blood is additionally cooled. This allows you to reduce the need for oxygen, and therefore the speed of blood flow. With particularly complex interventions, hypothermia can reach 15 degrees.
The effect of artificial blood circulation on the body
Hemodynamic conditions that are perceived by the body as stressful include:
- reverse blood flow in the aorta,
- minimum level of pressure in the cavities of the heart,
- destruction of blood cells during movement along rigid highways,
- shutdown of pulmonary blood flow,
- accumulation of pain mediators in the blood,
- hypotension and low vascular resistance.
An operation involving connection to a heart-lung machine is similar to severe injury, blood loss and shock. To compensate, the body redistributes nutrition in such a way as to protect the brain and heart to the detriment of other organs. This makes it difficult to achieve normal blood flow even at high perfusion rates. Therefore, tissues suffer from a lack of oxygen and metabolic acidification of the blood.
Three methods
In modern medicine, three extracorporeal circulation systems are used:
- general;
- regional;
- auxiliary
In the first case, the AIC completely replaces the lungs and heart. This method is practiced in cardiac surgery.
Regional blood circulation refers to the perfusion of a separate organ, which is isolated from the circulatory system for some time. This method is often used in purulent surgery and oncology in order to deliver a larger amount of drugs to the sore spot.
The main tasks of assisted circulation:
- reduce oxygen consumption by the myocardium;
- increase its oxygen supply;
- increase the supply of oxygen to other physiological systems or organs.
Basic operation of AIC