What is thrombocytopenic purpura in children?
Thrombocytopenic purpura (TP), or Werlhoff's disease , is a blood clotting disorder characterized by a decrease in the number of platelets in the blood.
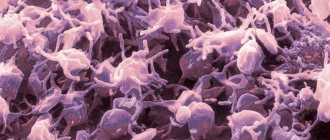
Platelets are cells in the blood that help stop bleeding. Their decrease leads to easy bruising, bleeding gums and internal bleeding.
The term "thrombocytopenia" refers to a decrease in the number of platelets in the blood, and "purpura" refers to the presence of purple spots and petechiae on the skin (hemorrhages) caused by internal bleeding from small blood vessels.
The disease is caused by an immune reaction to your own platelets.
Medications
Your doctor will discuss with you the side effects and dosage of the medications and dietary supplements you are currently taking. It is possible that some of them contribute to a decrease in the level of platelets in the circulating blood. Aspirin, Ibuprofen, Ginkgo biloba and Warfarin have such side effects.
Causes
Etiological factors
The exact cause of TP is unknown, so it is sometimes called idiopathic . The disease is not contagious, that is, a child cannot “catch” it while playing with other children with TP.
Often, a child may have a viral infection three weeks before developing TP. It is believed that the body, while creating antibodies against the virus, “accidentally” also produces an antibody that sticks to platelets.
The immune system identifies any cells with antibodies as foreign bodies and destroys them.
Helicobacter pylori infection is associated with autoimmune diseases, including TP; the pathology can also occur with HIV and other hematological disorders, including chronic lymphocytic leukemia, lymphogranulomatosis, and non-Hodgkin's lymphoma.
Genetic variations in several genes are found in some patients with LT and may increase the risk of developing abnormal immune responses. However, the contribution of these genetic changes to the development of immune thrombocytopenia is unclear.
There have been studies looking at some drugs that cause AFL . Some medications can cause changes in platelet function. At present, no direct link has been found to any specific drug that may cause AFL.
In newborns, LT can be caused by maternal antibodies transferred to fetal platelets. Differences in fetal and maternal platelet antigens can lead to the destruction of fetal platelets.
Predisposing factors for the development of chronic TP in children
They are:
- frequent and persistent bleeding observed six months before acute AFL;
- there is no connection between exacerbation and the impact of any provoking criteria;
- the patient has chronic foci of infection;
- development of TP in girls during puberty.
Prevention
Since the mechanisms and causes of Werlhof's disease have not been sufficiently studied at present, primary prevention means that could completely prevent the development of the disease have not been developed. Secondary prevention, aimed at preventing relapses and exacerbations of the disease, consists of:
- minimizing the risk of injury;
- avoiding contact with infectious patients;
- diet (exclude spicy foods, alcohol, caffeine);
- avoiding direct sunlight, solarium, and some physiotherapy procedures (UHF, UV radiation).
- exemption from physical education.
Werlhof's disease is a serious disease that can lead to various complications. Therefore, parents need to closely monitor the well-being of their child. If any symptoms appear, you should consult a doctor as soon as possible. Following the recommendations of a specialist will help keep your baby healthy.
Classification
| Criterion | Characteristic | ||
| Development mechanism | Heteroimmune, occurs when the antigenic structure of platelets is modified due to the influence of certain factors (viruses, new antigens, semi-antigens), characterized by an acute course | Autoimmune, occurs when autoantibodies are produced that attack their own unchanged platelets; characterized by a chronic, relapsing course | |
| Period | Exacerbations (crisis) | Remissions | |
| Clinical: no hemorrhages, but platelet count is reduced | Clinical and hematological – there are no clinical and laboratory signs of platelet deficiency | ||
| Severity of pathology | Mild: bruising and petechiae, occasional minor nosebleeds, very minor disruption of daily life | Moderate – more serious damage to the skin and mucous membranes, more profuse nosebleeds; platelet count 55 – 105 x 10*9 /l | Severe – long and heavy bleeding, skin manifestations, platelet level 35 – 55 x 10*9 /l, posthemorrhagic anemia, symptoms that seriously affect the quality of life |
| Flow | Acute (less than six months) | Chronic (more than six months): with rare relapses or regularly recurring | |
Kinds
TP is classified according to etiological, pathogenetic and clinical features. The classification reflects the cause of the disease and helps to find adequate treatment.
Pathology happens:
- idiopathic thrombocytopenic purpura (Werlhof's disease);
- symptomatic thrombocytopenia (Werlhoff symptom complex).
TP is also classified according to the nature of its course:
- Acute form. Usually seen in children. Lasts up to six months. After normalization of platelets, relapses are not observed.
- Chronic form. Lasts more than six months and is more common in adults. Refers to recurrent forms. Repeats cyclically. The platelet level is unstable. After normalization, platelet deficiency occurs.
Doctors use another classification of TP. It divides pathology into several immune forms:
- Isoimmune. It is usually observed after blood transfusions. There is also a congenital pathology. Develops due to an immune conflict with platelet antigens that occurs between the mother and fetus. The peculiarity of this clinical form is regular relapses.
- Autoimmune. It appears due to the fact that the body forms a lot of platelet antibodies to its own platelets.
- Heteroimmune. This form is usually provoked by taking medications. In this case, the individual sensitivity of the child is of great importance. Due to intolerance to certain substances contained in the drugs, children develop specific symptoms - purple rashes. They arise as a result of numerous hemorrhages.
- Transimmune. The development of this form is preceded by an antigenic conflict and the accumulation of antiplatelet antibodies during pregnancy. These antibodies, entering the child’s body through the placental bloodstream, cause the development of hemorrhagic syndrome.
Symptoms
Manifestations of purpura in newborns
A baby should be suspected of having TP if petechiae appear throughout the body soon after birth and blood tests show severe thrombocytopenia. Clinical manifestations may range from limited or widespread cutaneous petechiae or skin bruising to excessive bleeding or intracranial hemorrhage.
Manifestations in children
A previously healthy child suddenly develops generalized petechiae. Parents often state that the child felt fine the day before, but is now covered in bruises and purple spots. Bleeding from the gums and mucous membranes often occurs, especially with deep thrombocytopenia. There may be a previous viral infection 1-4 weeks before the onset of TP. Splenomegaly, lymphadenopathy (enlarged spleen and lymph nodes, respectively), bone pain and pallor are rare.
The presence of abnormal findings, such as hepatosplenomegaly (enlarged liver and spleen), bone or joint pain, or severe lymphadenopathy, indicates other diseases (eg, leukemia).
Manifestations in adults
In adults, chronic TP is often observed, which develops slowly.
Symptoms include:
- petechiae;
- bruising;
- bleeding from the nose and gums;
- black blisters in the mouth;
- fatigue;
- heavy menstrual periods in women.
Rarely, the following symptoms may occur:
- hemorrhages in the retina and brain;
- bleeding from the ears;
- blood in urine;
- bleeding in the intestines.
Forecast
In adults, thrombocytopenic purpura ends in complete recovery in 75% of cases, in children - in 90% of cases. The occurrence of serious complications is possible only in the acute period of the disease.
The likelihood of death with the thrombotic variant of thrombocytopenic purpura depends on the extent of the lesion and the degree of damage to the brain, cardiovascular system, kidneys and other organs.
Patients with a history of this pathology need constant medical supervision, exclusion of medications that negatively affect blood clotting, and a review of lifestyle and nutrition.
Diagnostics
To diagnose FL, you need to rule out other possible causes of bleeding and low platelet counts, such as an underlying medical condition or medications your child may be taking.
The specialist will need to take a medical history, perform a physical examination, and perform several laboratory tests.
Complete blood count
This test is used to determine the number of blood cells, including platelets, in a sample. In LT, the white blood cell and red blood cell counts are usually normal, but the platelet count is decreased.
Blood smear examination
This method is often used to confirm platelet levels found on a complete blood count. The blood sample is placed on a slide and examined under a microscope.
Bone marrow examination
This test helps determine the cause of a low platelet count, although some hematologists do not recommend this test for children with AFL.
In patients with LT, the bone marrow will be normal because the low platelet count is due to the destruction of these cells in the bloodstream and spleen, not due to abnormalities in the bone marrow.
Other studies
Blood testing for HIV should be carried out in risk groups, especially among sexually active adolescents. A direct antiglobulin test should be done if there is unexplained anemia to rule out Evans syndrome (autoimmune hemolytic anemia and thrombocytopenia).
Diagnostic measures
Suspicion of the presence of hemorrhagic syndrome arises when hemorrhages are detected on the child’s body. If bruises occur on their own, consult a pediatrician. An accurate diagnosis is made by another specialist - a pediatric hematologist.
To diagnose the disease, several studies and laboratory tests are performed.
Diagnostic tasks:
- find out what form of pathology is present in the child;
- determine the severity of physiological abnormalities.
Before sending a child for examination, the doctor analyzes the course and symptoms of the disease. Finds out how the pathology began, whether it was observed in blood relatives in early childhood. Then he examines the patient.
Treatment
The goal of care for a patient with AFL is to increase the platelet count to a safe level. There is no cure for TP, and relapses can occur years after seemingly successful medical or surgical treatment.
Drug therapy
Steroids
The use of steroids is the mainstay of treatment for this disorder. This group of drugs helps suppress the immune system. The route of administration and dosage is determined by the platelet count and the presence of any active bleeding. Intravenous infusions of methylprednisolone or dexamethasone may be given in emergency situations. For milder forms, oral forms of prednisolone can be used.
As the platelet count normalizes, the dosage of steroids is gradually reduced. Almost 60%-90% of patients experience relapses during dosage reduction or discontinuation. Long-term use of steroids is not recommended as it can cause various side effects.
Immunosuppressants
Immunosuppressants such as azathioprine and mycophenolate mofetil are becoming increasingly popular due to their effectiveness in treating LT. For chronic and persistent pathologies, when the immune pathogenesis has already been established, a chemotherapeutic agent, vincristine, can be used. However, the drug causes serious side effects and should therefore be used only with caution in the treatment of TP. This is especially important for children, as they are more vulnerable.
Immunoglobulin
This medicine contains antibodies that are a product of human blood, meaning that the antibodies were collected from multiple donors. It is not known exactly how the drug works to treat TP, but the additional antibodies are thought to stop white blood cells from destroying platelets. The drug works quite quickly, usually within a few days. Unfortunately, the effect does not last long (only a few weeks). Medicine is usually given before surgery, or if there is significant bleeding and platelet levels need to be increased urgently.
Rituximab
This drug was originally used to treat cancer, but it has also been used in the treatment of LT for almost 20 years. Like steroids, it stops the immune system from destroying platelets, but has fewer side effects than steroids. This is an artificially created antibody that affects white blood cells. It is not made from human donor blood. Effects are usually achieved within a few weeks, although some people respond to treatment after several months.
Thrombopoietin receptor agonists Romiplostim and Eltrombopag
These two drugs have become available in the last few years. Thrombopoietin receptors are found on the surface of the cells that make platelets in the bone marrow; these drugs use these receptors to tell the cell to make more platelets. The drugs can only be used in combination with other treatment methods. Romiplostim is used as a subcutaneous injection, usually once a week. Eltrombopag comes in tablet form that you take once a day. The substance is not absorbed by the intestines without calcium, so it is necessary to eat foods high in calcium within four hours before or after taking the drug.
Therapy should be continued until clinical and laboratory manifestations disappear; this may take several years. Medicines do not cure the underlying problem; they simply encourage the body to produce more platelets to replace those that are destroyed.
Treatment of Helicobacter Pylori
Some children with LT have a stomach infection called Helicobacter pylori. Sometimes treating her with antibiotics and antacids for two weeks can cure or improve TP. The increase in platelets after treatment of an infection is not always permanent, but the therapy is relatively safe and can therefore be recommended for children.
Dapsone
It is an antibacterial agent but can also be used to treat TP. It is not known exactly how the drug works, but it appears to reduce the autoimmune process, which may stop the immune system from attacking platelets. It is taken as a tablet once a day and has several side effects.
Tranexamic acid
This drug helps blood clots last longer once they form. The clots are more stable than usual and more persistent. The drug does not treat AFL, but may be useful for bleeding while the platelet count is low. The tablet is taken 3 or 4 times a day. There are contraindications.
Why shouldn't platelet transfusions be given?
The platelets produced by the bone marrow are healthy. Their low number is due to the immune system attacking them. If a patient receives platelets from a donor, they will be destroyed by your immune system. Platelet transfusions are useful as emergency treatment if there is severe bleeding, as they will help form a clot, but this method is not effective in preventing bleeding long-term.
Surgery
Because platelets are mostly destroyed while they are in the spleen, removing it (splenectomy) can cure the pathology. Splenectomy has been used to treat TP for decades and offers the best chance of cure. Of every three people who have surgery, two will not need further treatment.
Splenectomy results in a lifelong increased risk of sepsis from bacterial infection.
In children, the risk of bacterial sepsis after splenectomy is estimated at 1-2%. Many pediatricians recommend delaying surgery until children are 5 years old.
If a splenectomy is planned, the child should be vaccinated against Haemophilus influenzae 14 days before surgery. Also, children over two years of age must be vaccinated against Streptococcus pneumoniae and meningococcal infection.
Diet
Diet plays a role in the treatment of TP. Eating the right foods will help your child feel better and more energetic.
Some nutrients, such as vitamin K and calcium, have natural components that are important for blood clotting. They are rich in dark leafy greens (spinach). Dairy products contain a lot of calcium, but experts do not recommend consuming it in excess, as it can worsen the symptoms of autoimmune diseases. Vitamin D supplementation also plays a role in boosting the immune system in LT.
Tips for organizing meals are as follows:
- If possible, it is recommended to consume only natural products;
- animal and artificial fats should be replaced with vegetable ones;
- it is necessary to limit the consumption of red meat;
- Potentially antiplatelet fruits such as berries, tomatoes and grapes should be avoided.
Recommendations for parents
If a child has TP, parents need to learn how to best prevent injury and bleeding:
- For a small child, make the environment as safe as possible. Padding the bed with soft materials, helmets and protective clothing are necessary when the platelet count is low;
- contact sports, cycling and rough play should be limited;
- Avoid medications containing aspirin because they may interfere with the body's ability to control bleeding;
- Until recovery from illness, the child should not receive vaccinations, especially those containing live attenuated viruses. These include measles, mumps, rubella, and oral polio vaccines. In addition, you should not inject into a muscle.