How does blood clotting occur?
The value of blood lies in its unique ability to deliver nutrition and oxygen to all organs, ensure their interaction, and evacuate waste waste and toxins from the body.
Therefore, even a small loss of blood becomes a health threat. The transition of blood from a liquid to a jelly-like state, that is, hemocoagulation begins with a physicochemical change in the composition of the blood, namely, with the transformation of fibrinogen dissolved in plasma.
What substance is dominant in the formation of blood clots? Damage to blood vessels is a signal specifically for fibrinogen, which begins to transform, turning into insoluble fibrin in the form of threads. These threads, intertwined, form a dense network, the cells of which retain the formed elements of the blood, creating an insoluble plasma protein that forms a blood clot.
Subsequently, the wound closes, the clot becomes denser due to the intensive work of platelets, the edges of the wound are tightened and the danger is neutralized. The clear yellowish liquid released when a blood clot hardens is called serum.
Blood clotting process
To more clearly imagine this process, we can recall the method for producing cottage cheese: coagulation of the milk protein casein also contributes to the formation of whey. Over time, the wound resolves due to the gradual dissolution of fibrin clots in nearby tissues.
Blood clots or clots formed during this process are divided into 3 types:
- White thrombus formed from platelets and fibrin. Appears in injuries with high blood flow, mainly in arteries. It is called so because the blood clot contains trace amounts of red blood cells.
- Disseminated fibrin deposits form in very small vessels, capillaries.
- Red blood clot. Clotted blood appears only in the absence of damage to the vascular wall, with slow blood flow.
Types of hemophilia
Based on the type of disorders to which the coagulation system may be susceptible due to mutation of the X chromosome, 3 types of hemophilia (the name of the disease with incoagulability of blood) can be distinguished:
- Type A. Occurs in most cases (up to 85% of diseases). With this variant of hemophilia, there is a deficiency of factor VIII, which causes problems in the synthesis of thrombokinase.
- Type B (or Christmas disease). Caused by insufficient synthesis of factor IX. This factor is also responsible for the synthesis of thrombokinase, but also for the production of secondary coagulating plugs. The frequency of occurrence for this type is 13%.
- Type C. This type of hemophilia can be found in only 2% of diagnosed patients. The key feature is that not only men, but also women are affected by the dominant type of disease. Type C is determined by a lack of thromboplastins, for which factor XI is responsible. It is important to note that some nations are more susceptible to this type of disease. First of all, this concerns Ashkenazi Jews.
In modern discussions about hemophilia and its classifications, the question has arisen as to whether type C should be included in the general list of varieties of the disease. The majority came to the conclusion that this subspecies is too different from types A and B in its manifestations, which means it must be excluded from it.
What is involved in the clotting mechanism?
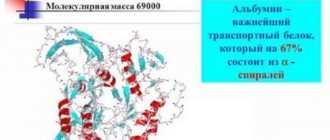
The most important role in the coagulation mechanism belongs to enzymes. This was first noticed in 1861, and the conclusion was made that the process could not occur in the absence of enzymes, namely thrombin. Since coagulation is associated with the transition of fibrinogen dissolved in plasma into the insoluble protein fibrin, this substance is the main one in the coagulation process.
Each of us has thrombin in a small amount in an inactive state. Its other name is prothrombin. It is synthesized by the liver, interacts with thromboplastin and calcium salts, turning into active thrombin. Calcium ions are present in the blood plasma, and thromboplastin is a product of the destruction of platelets and other cells.
To prevent the reaction from slowing down or not completing, the presence of the most important enzymes and proteins is necessary in a certain concentration.
For example, the well-known genetic disease hemophilia, in which a person is debilitated by bleeding and can lose a dangerous amount of blood due to one scratch, is due to the fact that the blood globulin involved in the process does not cope with its task due to insufficient concentration.
Blood clotting mechanism
Causes of the disease
The causes of increased blood clotting are very diverse and can be caused by many factors. Here are the main ones:
- infectious diseases;
- hormonal diseases;
- diseases of internal organs (liver, spleen);
- pregnancy;
- slow blood flow due to lack of physical activity;
- atherosclerosis;
- genetic pathologies of hemostasis;
- dehydration of the body;
- irradiation;
- autoimmune diseases;
- metabolic disorder.
As a result of these diseases, the chemical composition and viscosity of the blood plasma is disrupted, which leads to a change in the normal state of red blood cells and platelets. These cells begin to intensively stick together, the ratio of the liquid part and the cellular mass of the blood is disrupted, and the risk of thrombus formation in the blood vessels and heart increases. Therefore, increased blood clotting is a serious health threat that requires immediate and competent treatment.
Why does blood clot in damaged vessels?
The process of blood clotting consists of three phases passing into each other:
- The first phase is the formation of thromboplastin. It is he who receives the signal from damaged vessels and triggers the reaction. This is the most difficult stage due to the complex structure of thromboplastin.
- Conversion of the inactive enzyme prothrombin into active thrombin.
- The final phase. This stage ends the formation of a blood clot. Thrombin acts on fibrinogen with the participation of calcium ions, resulting in fibrin (an insoluble thread-like protein), which closes the wound. Calcium ions and thrombostenin protein compact and secure the clot, resulting in retraction of the clot (reduction) by almost half in a few hours. Subsequently, the wound is replaced with connective tissue.
The cascade process of thrombus formation is quite complex, since a huge number of different proteins and enzymes are involved in coagulation. These necessary cells (proteins and enzymes) involved in the process are blood coagulation factors, a total of 35 of them are known, of which 22 are platelet and 13 are plasma.
Factors contained in plasma are usually designated by Roman numerals, and platelet factors by Arabic numerals. In the normal state, all these factors are present in the body in an inactive state, and with vascular damage, the process of their rapid activation begins, resulting in hemostasis, that is, stopping bleeding.
Plasma factors are protein in nature and are activated during vascular damage. They are divided into 2 groups:
- Dependent on vitamin K and produced only in the liver,
- Vitamin K independent.
Factors can also be found in leukocytes and erythrocytes, which determines the enormous physiological role of these cells in blood coagulation.
Clotting factors exist not only in the blood, but also in other tissues. The thromboplastin factor is contained in large quantities in the cerebral cortex, placenta, and lungs.
Platelet factors perform the following tasks in the body:
- Increase the rate of thrombin formation,
- Promote the conversion of fibrinogen into insoluble fibrin,
- Dissolving a blood clot
- Promotes vasoconstriction
- Take part in the neutralization of anticoagulants,
- They promote the “gluing” of platelets, due to which hemostasis occurs.
Methods for diagnosing blood clotting
There are several ways to determine how long it takes for a wound to heal. The Fonio method is widely used in clinical practice. The test physiological fluid is collected from a vein, the material is applied to a glass plate, which is placed in a chamber with high humidity. A Pasteur pipette is passed over the surface of the blood. The fact that the coagulation process begins can be judged by the fibrin strands that are formed, which stretch behind the glass rod. The end is when a clot forms. The norm is the appearance of fibrin threads after 5-8 minutes from the start of testing, and a clot after 15-18.
Attention ! The clotting test is carried out not only before operations. A deviation from the norm indicates pathological changes in the human body.
If the Lee-White method is used, blood is drawn from a vein. Then the sample is divided into 4 portions and placed in test tubes that are installed in a water bath at 37°C. The tubes are rotated every 30 seconds until the blood clots and separates from the walls. Estimate the time for each test tube, calculate the average value, taking it as the final result. The norm is 6-10 minutes.
With the Jacques-Fiedler-McDonald method, studies are similar to Lee-White, but laboratory glassware made of silicone is used to assess coagulation.
These are not the only ways to study hemostasis. Can be used:
- Brucker method: sampling is made from a finger. Place on glass until fibrin forms, mixing the sample with a drop of distilled water;
- Mas-i-Magro method: blood is taken from a finger. The test sample is combined with petroleum jelly and checked for the formation of fibrinogen by how long it takes to draw the substance into the pipette (drying rate is 8-12 minutes);
- Sitkovsky-Egorov method: analysis requires a special device with a chamber for pressurizing.
The clotting test is called a coagulogram or hemostasiogram. During the study, several indicators are determined at once:
- coagulation time - the interval from the moment artificially induced bleeding begins until it stops;
- prothrombin index - shows how coagulability in the sample differs from that of a healthy person;
- thrombin time - the interval of conversion of fibrinogen protein into fibrin;
- activated partial thromboplastin time - when a clot forms;
- activated recalcification time - this value can be used to judge the rate of decrease in the number of platelets;
- fibrinogen concentration - shows the functioning of the liver, pancreas, exacerbation of infectious processes in the body;
- fibrinolytic activity - the ability to dissolve blood clots.
Attention ! It is very important that the tests are interpreted by a specialist. The processes occurring in the body must be judged by a set of values, and not just by one indicator.
Blood clotting normal over time
One of the main blood indicators is a coagulogram - a study that determines the quality of clotting. The doctor will always refer you for this study if the patient has thrombosis, autoimmune disorders, varicose veins, acute and chronic bleeding of unclear etiology. This analysis is also needed for necessary cases during surgery and pregnancy.
The blood clot test is performed by drawing blood from a finger and measuring how long it takes for the bleeding to stop. The coagulation rate is 3-4 minutes. After 6 minutes it should already be a gelatinous clot. If blood is extracted from the capillaries, a clot should form within 2 minutes.
Children have faster blood clotting than adults: the blood stops after 1.2 minutes, and a blood clot forms after only 2.5-5 minutes.
Also important when testing blood are the following measurements:
- Prothrombin is a protein responsible for coagulation mechanisms. Its norm: 77-142%.
- Prothrombin index: the ratio of the standard value of this indicator to the patient’s prothrombin value. Norm: 70-100%
- Prothrombin time: the period of time during which clotting occurs. For adults it should be within 11-15 seconds, for small children 13-17 seconds. It is a diagnostic method for suspected hemophilia and DIC syndrome.
- Thrombin time: shows the rate of thrombus formation. The norm is 14-21 seconds.
- Fibrinogen is a protein responsible for the formation of blood clots, indicating existing inflammation in the body. Normally, it should be 2-4 g/l in the blood.
- Antithrombin is a specific protein substance that ensures the resorption of a blood clot.
Symptoms of increased clotting
With increased blood clotting, doctors recommend drinking at least 1.5 - 2 liters of juice per day.
Mainly, symptoms of increased blood clotting manifest themselves in a feeling of constant fatigue, a feeling of heaviness in the legs. Patients quickly get tired when walking, experience weakness, drowsiness, and headaches of varying intensity.
Symptoms of thrombophilia manifest themselves in the form of bruises that appear on the body with minor injuries and bruises. This is due to the high fragility of microvessels. Patients experience increased gum bleeding. Disruptions occur in the functioning of the intestines and internal organs, the tissues of which are poorly supplied with oxygen and nutrients. Hemorrhoids become painful and swollen.
High blood clotting leads to thrombosis and varicose veins, the symptoms of which are spider veins and venous nodes in the legs. Symptoms of high blood viscosity most often appear in diseases such as obesity, diabetes, stress, smoking, cancer and autoimmune diseases.
The dangers of increased blood viscosity during pregnancy
Currently, doctors are increasingly talking about the connection between thrombophilia and complications that arise during pregnancy. Increased blood clotting during pregnancy can result in miscarriage. In pregnant women, the tendency to form blood clots increases many times over. Moreover, in women who have increased blood viscosity before conception, the problem worsens during pregnancy. The result can be various complications: late toxicosis, miscarriage, placental abruption, premature birth and even intrauterine fetal death.
How do these complications arise? The unborn child receives all the vital substances it needs from the placenta, which has many blood capillaries and vessels. If blood clots form at the junction of the placenta with the uterus or in its blood vessels, the fetus cannot receive nutrients and stops developing.
Using modern techniques, women are identified who suffer from high blood viscosity, who are prone to the formation of blood clots, and who have suffered complications during pregnancy in the past. To prevent possible problems, they are treated with blood thinners.
Treatment for increased blood clotting
When treating high blood viscosity, special attention should be paid to the causes of its occurrence and diagnosis.
The classic treatment for thrombophilia is taking anticoagulants. Depending on the nature of the pathology, antispasmodics, anti-inflammatory drugs, and fibrinolytics may be prescribed. A procedure may be used to replenish blood volume using transfusion and infusion therapy, or a method of removing blood clots through surgery may be used.
For hereditary thrombophilias, long-term use of aspirin in small doses is indicated. During pregnancy, aspirin is contraindicated. Treatment should be carried out with constant laboratory monitoring of blood counts, since uncontrolled internal bleeding can easily occur when taking blood thinning drugs. All medications should be taken only as prescribed by the attending physician and under his supervision.
Under what conditions is equilibrium between two inverse systems maintained?
In the human body, two systems operate simultaneously to ensure coagulation processes: one organizes the rapid onset of thrombus formation in order to reduce blood loss to zero, while the other in every possible way prevents this and helps maintain the blood in the liquid phase. Often, with certain health problems, pathological blood clotting occurs inside intact vessels, which is a great danger, significantly exceeding the danger from bleeding. For this reason, thrombosis of the blood vessels of the brain, pulmonary artery and other diseases occur.
It is important that both of these systems work correctly and are in a state of intravital equilibrium, in which the blood will coagulate only when the vessels are damaged, and inside the undamaged ones will remain liquid.
Factors that cause blood to clot faster
- Painful irritations.
- Nervous excitement, stress.
- Intensive production of adrenaline by the adrenal glands.
- Increased levels of vitamin K in the blood.
- Calcium salts.
- Heat. It is known at what temperature a person’s blood clots – at 42 degrees C.
Factors that prevent blood clotting
- Heparin is a special substance that prevents the formation of thromboplastin, thereby stopping the coagulation process. Synthesized in the lungs and liver.
- Fibrolysin is a protein that promotes the dissolution of fibrin.
- Attacks of severe pain.
- Low ambient temperature.
- Effects of hirudin, fibrinolysin.
- Taking potassium citrate or sodium.
If you suspect poor blood clotting, it is important to identify the causes of the situation, eliminating the risks of severe disorders.