Currently, arrhythmias are quite common. There are frequent cases of their combination with hypotension (low blood pressure), which aggravates the condition of patients and requires an integrated approach to diagnosis and treatment. It is important to understand that there are a large number of different types and forms of arrhythmias that have completely different causes. Any disruption of the heart is a serious symptom; they can be classified as so-called “red signs”, especially if we are talking about an acute arrhythmia, which is accompanied by a decrease in blood pressure. Therefore, the answer to the question: “I have arrhythmia and low blood pressure, what should I do?” – there will be a timely request for help from a specialist: family doctor, therapist, cardiologist.
Reasons for development
Arrhythmia (extrasystole) is manifested by a violation of the heart rhythm. The following reasons contribute to its development:
- hypertension;
- smoking;
- alcohol abuse;
- diabetes;
- excessive caffeine consumption;
- pathologies of the heart valves;
- stress;
- taking certain medications;
- drug overdose;
- food poisoning;
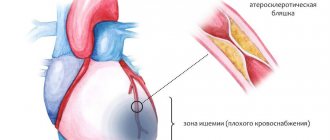
- ischemic disease;
- electrolyte disturbances;
- cardiomyopathy.
The following conditions lead to arrhythmia:
- damage to the heart muscle;
- poor blood supply. Reduced blood flow to the heart changes the ability of cells to form and conduct electrical impulses;
People at risk for developing heart pathologies include:
- thyroid diseases;
- hereditary predisposition;
- congenital heart abnormalities.
To avoid problems with the heart and blood vessels, it is recommended to minimize the influence of provoking factors.
People who are at risk of developing such pathologies should be especially attentive to their health.
How to prevent this condition from occurring?
Prevention of arrhythmia and hypotension is quite simple, but its effectiveness can significantly increase the chances of improving health and avoiding the development of such conditions.
For functional hypotension that is not accompanied by diseases and changes in the structure of the heart, preventive measures include:
- maintaining an active lifestyle;
- moderate physical activity;
- full healthy sleep;
- sufficient consumption of vitamins necessary for the body at different times of the year;
- giving up bad habits and following a diet.
In the presence of serious heart pathologies, the prevention of arrhythmia will be more focused on maintaining the cardiovascular system in order, which significantly reduces possible physical stress on the body.
Arrhythmia occurring with a decrease in blood pressure is a serious cause for concern. Such symptoms require timely seeking qualified medical help. If this is not done, you can cause irreparable harm to health, even death. But with proper treatment, stabilization of the patient’s condition will not take much time, and his health will quickly improve.
Why does blood pressure increase?
Hypertensive patients are susceptible to heart contraction disorders. With constantly elevated blood pressure, the volume of the left ventricle increases due to excess blood ejection.
Failure of this part of the heart causes arrhythmia. With high numbers on the tonometer, the pulse is usually rapid.
A pathological increase in heart rate provokes the formation of additional sources of excitation in the muscle fibers of the heart, which send impulses, causing short-term interruptions in muscle function. This leads to extrasystole.
The combination of extrasystole and hypertension is often observed in elderly people. This is due to the deterioration of blood vessels and wear and tear of the heart muscle.
Arrhythmia may also develop against the background of a hypertensive crisis. In this case, increased pressure is combined with acute left ventricular failure. The pulse quickens and the activity of the heart is disrupted.
Low blood pressure with high heart rate
To find the reason why arrhythmia began with low blood pressure, the patient needs to be examined by several doctors.
In this condition, the patient's pulse often increases. It is worth visiting a cardiologist, therapist, neurologist. It is necessary to undergo a series of tests to determine the exact cause. A number of the main reasons include blood loss, states of shock, overdose and poisoning of medications, deviations or malfunctions of the endocrine system, pathologies of the vegetative-vascular system, and pregnancy. A condition in which arrhythmia develops and low blood pressure is accompanied by pain in the chest, heart and head. Low blood pressure coupled with a high heart rate provokes nausea and vomiting. When blood pressure drops sharply, patients feel anxiety, weakness, dizziness, and are haunted by a feeling of fear.
Treatment of the disease
Pulse and blood pressure should be measured regularly using a tonometer.
Regularly measure your pulse and blood pressure using electronic tonometers.
If your heart rate is often abnormal when your blood pressure is low, consult a doctor. Only he will select the appropriate drug. Most medications that normalize the pulse lower blood pressure, which is unacceptable in low blood pressure. To begin with, it is recommended to take soothing infusions such as valerian. Patients must give up their unhealthy lifestyle and bad habits. It is recommended to raise blood pressure by adjusting the diet and taking vitamin complexes.
Diagnosis
Quite often, an accurate description of the symptoms helps the doctor more accurately make a diagnosis, as well as determine the severity of the disease. The medical professional always asks the patient to describe the contractions of the heart muscle in as much detail as possible. In particular, how fast/slow, short/long, regular/irregular, etc. are they. It is also important to know in what physical state severe palpitations occur.
To determine a more precise cause of arrhythmia in conditions of high or low blood pressure, additional research is needed. The main one is electrocardiography. It is this method that records the electrical activity of the heart muscle. An ECG provides data over a short period of time. And to obtain more accurate information, Holter monitoring is carried out. In addition, the patient should keep a diary of symptoms that make themselves felt over a certain period of time. If during the examination it was discovered that there is a threat to the patient’s life, then he must be hospitalized.
call me back
Description of hypertensive arrhythmia
Arrhythmia should be understood as a disturbance of normal cardiac activity, which is expressed in a regular sinus rhythm. The pathogenesis of the disease consists of both a violation of the conductivity of the electrical impulse and the presence of organic disorders in the heart muscle. The last variant of the development mechanism is most typical for hypertensive arrhythmia.
Read also: Persistent form of atrial fibrillation
Hypertension is a very insidious disease, since in the process of its development it affects many different so-called target organs: kidneys, optic nerve, vascular system of the brain and heart. Therefore, during hypertension the following is observed:
- initially high cardiac output;
- myocardial damage as a result of revascularization of the coronary arteries.
As a result of such processes, the heart muscle compensates for the negative effects of high blood pressure for a certain period of time. After resources are used up, heart failure and hypertensive arrhythmia begin to appear in this case, one might say, the “first sign” of further complications.
The appearance of hypertensive arrhythmia is an unfavorable sign that indicates the initial development of organic lesions of blood vessels and cardiac tissue.
Arrhythmia with normal blood pressure and pulse
In a healthy person at rest, the heart contracts at a rate of 60 to 100 beats per minute. Rhythm disturbances with normal blood pressure can occur for various physiological reasons and be a manifestation of a disease.
Arrhythmia with normal tonometer numbers is observed when:
- pregnancy;
- high body temperature;
- physical activity;
- lack of oxygen in the room;
- anemia;
- thyrotoxicosis;
- pathologies of the lungs that occur with impaired gas exchange;
- vegetative-vascular dystonia. Usually, health worsens due to stress and weather changes.
Arrhythmia with normal blood pressure also occurs in some heart diseases:
- myocarditis;
- mitral valve disease;
- myocardial infarction;
- chronic pulmonary heart disease;
- pericarditis;
- aortic insufficiency.
A decrease in blood sugar can lead to extrasystole. Therefore, insulin-dependent diabetics need to carefully monitor their diet.
Types of arrhythmias that occur with hypertension
It can manifest itself in various forms, some of which are more dangerous for their complications than others. We present, in order of increasing severity and severity of the clinical picture, the following arrhythmias, which most often occur with hypertension:
Sinus tachycardia
With this pathology, a rapid heartbeat is observed while maintaining sinus rhythm. Heart rate is 90 times or more per minute. With a sharp increase in blood pressure, which is often observed during a hypertensive crisis, an attack of tachycardia occurs, which in mild cases goes away on its own. If heart failure develops against the background of hypertension, then sinus arrhythmia may be permanent.
Extrasystole
It manifests itself as a feeling of “interruption” or as a strong blow behind the sternum. Visible on the ECG as a premature contraction. A single extrasystole is safer, which in difficult cases can become paired and polymorphic. When it occurs frequently, it significantly worsens coronary blood flow, which in hypertension does not function at 100%.
The location of extrasystole (in the ventricles, atria, atrioventricular node, sinus node) also plays a role in the development of the clinical picture. The most dangerous are those hypertensive arrhythmias that develop in the ventricles, since then hemodynamics are most quickly disrupted. Basically, with extrasystole, the prognosis is favorable, unless significant organic damage to the heart occurs.
Paroxysmal tachycardia
Attacks of rapid heartbeat with a heart rate from 150 to 280 times per minute. Characterized by a sudden onset and end of attacks. It can occur in various parts of the heart, therefore atrial, ventricular and atrioventricular paroxysmal tachycardia are distinguished. Associated with a disturbance in the conduction of electrical impulses; in some cases, organic changes in the myocardium are noted.
In mild stages, manifestations go away on their own. Or, to relieve an attack, the vagus nerve is stimulated. To do this, the area of the carotid sinus is rubbed with massage movements or a sharp exhalation is made. If the above actions are insufficiently effective, anaprilin is taken or injectable isoptin is administered. In severe cases, electrical pulse treatment may be required.
Cardiac blockades
They represent a disorder of the conduction system of the heart, in which complete or partial dysfunction of individual parts of the organ develops. Often associated with organic disorders occurring in the myocardium against the background of hypertension.
Read also: Atrial fibrillation treatment tablets
Heart blocks are clearly visible on the electrocardiogram. Depending on the location of the cause of the disorder, complete atrioventricular, sinoauricular, and intraatrial blockades are distinguished. The most dangerous type of blockade is complete, since the heart begins to contract chaotically, which negatively affects hemodynamics.
Atrial fibrillation
An unfavorable rhythm disturbance, accompanied by contraction of the atria over 300 times a minute, and the ventricles - 200 times a minute. In this case, the heart rate can reach 500 times per minute. There are various forms of the disease - paroxysmal, persistent, long-term persistent and permanent. Each of them can occur in hypertension.
Recent studies have shown that atrial fibrillation develops in 5% of people after 60 years of age. It is this category of the population that is at risk for hypertension, so these two pathologies are often combined in the clinic. The most dangerous is the permanent form of AF, which is more likely than others to develop into ventricular fibrillation. Pathology also increases the risk of developing vascular thromboembolism and stroke.
Atrial and ventricular fibrillation.
A life-threatening condition in which chaotic, irregular and very frequent heartbeat develops. The atria and ventricles work differently, causing the heart to stop performing its functions. As a result, the entire body begins to feel an acute lack of oxygen.
In hypertension, this complication, along with stroke, is one of the most dangerous. It develops mainly in the last stages of the underlying disease. Self-resolution rarely occurs, so emergency medical attention is needed.
Symptoms
Cardiac arrhythmia develops in a latent form. Therefore, at the beginning it does not manifest itself in any way. Only a doctor can detect pathology during an ECG procedure.
As the disease progresses, unpleasant symptoms begin to appear, indicating brain tumors, cardiac ischemia, hypertension or thyroid pathologies.
The following signs are characteristic of arrhythmia:
- dyspnea;
- darkening of the eyes;
- dizziness;
- general weakness;
- fast fatiguability;
- loss of consciousness;
- a feeling of either speeding up or slowing down the pulse;
- pressing pain in the chest.
If the symptoms described above appear, you should contact the clinic. Timely diagnosis and treatment will help reduce the likelihood of complications to a minimum.
Symptoms of the disease
| What is the pressure | Symptoms |
| High blood pressure | There is noise in the ears and head, a headache that appears as a pulsation in the temporal zone. Shortness of breath and shortness of breath, pain in the heart area. Persuaded by feelings of fear and anxiety. |
| Low blood pressure | A decrease in blood pressure provokes weakness, dizziness, nausea and vomiting. Fainting and noise in the head and ears occur. Oxygen starvation leads to headaches and shallow breathing. Such people have increased sweating and uneven, rapid breathing. |
Local anesthetics - when to use them
Drugs for local anesthesia (Lidocaine and Novocainamide) in addition to the anesthetic effect have an antiarrhythmic effect. It is most pronounced in relation to the ventricles of the heart. None of the existing drugs for the treatment of arrhythmia has a similar effect.
Both Novocainamide and Lidocaine are available only in injection form. They are administered intravenously in exceptional cases for ventricular arrhythmias - ventricular fibrillation and fibrillation, frequent ventricular extrasystoles. They act immediately after administration, but only for a short time. They are effective, but not without side effects in the form of allergic reactions.
Sources
- https://VseOSerdce.ru/hpc/arrhythmia/aritmiya-pri-nizkom-davlenii.html
- https://heal-cardio.ru/2015/10/13/ponizhennoe-davlenie-i-aritmija/
- https://www.vzdorovomtele.ru/lechenie-aritmii-serdca/lekarstva-ot-davlenija-pri-aritmii.html
- https://www.vzdorovomtele.ru/lechenie-aritmii-serdca/aritmija-pri-nizkom-davlenii-lechenie.html
- https://nashedavlenie.ru/gipotenziya/aritmiya-i-nizkoe-davlenie.html
- https://okardio.com/aritmiya/antiaritmicheskie-preparaty-088.html
What should be the pressure for atrial fibrillation?
Arterial hypertension as a factor of high cardiovascular risk is one of the pressing medical and social problems both in Russia and in countries with developed economies. It is associated with a high risk of cardiovascular events, widespread prevalence and insufficient control throughout the population. Large multicenter studies have convincingly shown that lowering blood pressure leads to increased life expectancy. This is confirmed by the real increase in life expectancy in Western countries. The significance of the problem is reflected in the 2004 Russian recommendations for the prevention, diagnosis and treatment of hypertension [1,2]. It is known that the relationship between the risk of stroke and blood pressure is more pronounced than for the risk of developing coronary heart disease. The risk of stroke is increased in the presence of possible sources of embolism in the heart (including atrial fibrillation, valve disease, etc.). Atrial fibrillation (or atrial fibrillation) is the most important source of thromboembolism due to its prevalence, relatively high risk of stroke, and causation in many cases. [3,5].
Atrial fibrillation (AF) is the most common rhythm disorder in the general population. Recently, it has been the subject of increasing interest and intensive study. The frequency of MA in people under 50 years of age is 0.2%; MA is somewhat more common in men than in women. With age, its frequency increases and amounts to 2-5% at the age of over 60 years and more than 10% at the age of 80-89 years [4]. The risk of death with AF is 2 times higher than with persistent sinus rhythm.
Accuracy of blood pressure measurement plays an important role in the diagnosis and monitoring of treatment of hypertension. The determination of blood pressure in a doctor’s daily practice is based on the auscultatory picture when measuring blood pressure with a sphygmomanometer (less commonly, a mercury one). The measurement technique is quite simple: you need to quickly inflate the air into the cuff to a pressure level of 20 mmHg. exceeding SBP (i.e. until the pulse disappears); then it is necessary to reduce the pressure in the cuff by 2 mm Hg. per second. The level of systolic pressure (SBP) corresponds to the pressure at which 1 sound appears (1st phase of Korotkoff sounds); The level of diastolic pressure corresponds to the pressure at which the sounds disappear (phase 5 of Korotkoff sounds). The presence of atrial fibrillation may make it difficult to determine phase 5 due to the initial attenuation of sounds due to the arrhythmia. Even more difficult is measuring blood pressure at home in this category of patients. Self-monitoring of blood pressure by patients and their relatives is an extremely important and necessary element in assessing the correctness and adequacy of hypertension treatment, which is reflected in all educational programs on hypertension. At home, automatic and semi-automatic devices are currently widely used to measure blood pressure, the measurement results of which can give a significant error, especially when measuring blood pressure on the forearm and on the fingers due to the inaccuracy of the obtained values. This problem is especially relevant for patients suffering from arrhythmias, especially atrial fibrillation, in whom all automatic oscillometric tonometers, as well as 24-hour blood pressure monitors, produce a systemic error, since they use pulse wave detection, and in patients with atrial fibrillation the pulse waves are non-rhythmic.
The emergence of a fundamentally new automatic device for measuring blood pressure in patients with arrhythmias, Tensoval duo control (“PAUL HARTMANN” Germany), is a new stage in self-monitoring of blood pressure in this severe category of patients. The innovative Duo Sensor Technology used combines two professional measurement technologies: first of all, auscultatory highly accurate Korotkoff technology and, as an additional option, oscillometric (pulse wave determination). Blood pressure is measured on the upper arm. A highly sensitive, interference-proof microphone is built into the device, which is equivalent to a doctor measuring blood pressure by listening to Korotkoff sounds with a stethoscope. In cases of a weak audio signal, this technology additionally connects an oscillometric measurement.
The device was tested in the UK at King's College, University of London, Thomas Hospital, carried out according to the British Hypertension League protocol (85 patients), the Tensoval Duo Control tonometer received an A/A rating. According to the data obtained, the average difference between the values of the Tensoval Duo Control tonometer and the standard (mercury sphygnomanometer) was 2.2 mm Hg. and 0.4 mm Hg. for systolic and diastolic values, respectively. This study involved 85 patients with arrhythmias (in 19 patients (22.3%) heart rate Cardiac Tensoval control, blood pressure, atrial fibrillation
The human body experiences different situations. One of them is when the heart beats in the chest like a bird, then trembles like an autumn leaf, and if it still beats and then freezes, then this is definitely an arrhythmia. In this case, heart contractions become irregular and irregular. There are several types of this disease, but there is one - the most common - atrial fibrillation. Each contraction is separated by approximately equal intervals and the person does not feel the work of the heart. At rest, 60-90 heart beats per minute is considered normal. If there are irregular contractions and different heart rates, we can already talk about arrhythmia. It is often noted that the pressure during atrial fibrillation is significantly increased.
As already mentioned, this disease is expressed by a violation of the following indicators: frequency, rhythm, sequence of compression of each of the chambers of the heart. And the reasons for this are:
- smoking and alcohol abuse;
- addiction to coffee;
- too much physical activity;
- insufficient or excess potassium in the heart;
- disease of the nervous system, on which the interaction of systems and organs depends;
- diabetes mellitus;
- disruptions in metabolic processes;
- curvature of the spine, as well as stress, depression, emotional shock and mental.
In addition to all this, diseases and defects of the heart muscle of congenital origin are important, and this also applies to the circulatory system and digestive organs. You must always understand that each case is individual, and the real cause can most likely only be determined by a qualified doctor. This is followed by the appointment of adequate therapy.
Most qualified medical staff are convinced that it is quite difficult for a person to feel any changes in the heartbeat. But most likely, this opinion is due to the fact that the average person is simply not aware of what these or other changes mean. Surely it would not hurt anyone to learn about the main signs that are characteristic of arrhythmia.
As a rule, the pressure during arrhythmia decreases, and accordingly, weakness and dizziness are felt. Moreover, it is possible to acquire a pre-fainting state, which you can think about if your eyes get dark during the slightest movement or change of position. It is noted that uncharacteristic changes in the functioning of the heart entail a chain reaction of the body as a whole.
For example, due to untimely, insufficient oxygen saturation of the blood, breathing occurs unevenly. And inadequate oxygen enrichment of all structural and elementary units of the body leads to strange noises in the head and pain under the rib on the left side, which are also signs of arrhythmia.
The situation is more serious with people who suffer from a congenital type of heart or circulatory system pathology. If arrhythmia occurs at low pressure, the patient can easily faint, and there is also an increased level of sweating and a feeling of catastrophic lack of air.
Along with the inhibition of heart contractions, uneven breathing is noted, general weakness and the skin turns pale.
All symptoms are long-term and of a sluggish nature. In this regard, people often simply ignore them, but it is arrhythmia that in most cases contributes to cardiac arrest, and as a result, the death of the patient.
It is noteworthy that, despite the fact that arrhythmia does not cause virtually any discomfort, it is, in fact, a very life-threatening illness.
There are many cases where people suffering from chronic high blood pressure begin to experience disruptions in the heart rhythm. This is due to the fact that under conditions of initially high cardiac output and the course of the disease, the left ventricle of the heart enlarges for a long time. And in most patients, the first consequence of high blood pressure is heart rhythm disturbances.
Arrhythmia, high blood pressure is usually caused by the presence of extrasystole, as well as paroxysmal tachycardia. The fact is that untimely depolarization and contraction of the heart occurs due to the formation of sources of additional excitation. They, in turn, send impulses. Under such conditions, the patient may feel a short-term cardiac arrest, and then a strong blow.
Failures of contractions in conditions of hypertension are very dangerous in their consequences. We can say that this sign indicates the acquisition of an extreme stage of this disease, and, accordingly, a modification of the blood vessels and organs of an organic nature.
Quite often, an accurate description of the symptoms helps the doctor more accurately make a diagnosis, as well as determine the severity of the disease. The medical professional always asks the patient to describe the contractions of the heart muscle in as much detail as possible. In particular, how fast/slow, short/long, regular/irregular, etc. are they. It is also important to know in what physical state severe palpitations occur.
To determine a more precise cause of arrhythmia in conditions of high or low blood pressure, additional research is needed. The main one is electrocardiography. It is this method that records the electrical activity of the heart muscle. An ECG provides data over a short period of time. And to obtain more accurate information, Holter monitoring is carried out. In addition, the patient should keep a diary of symptoms that make themselves felt over a certain period of time. If during the examination it was discovered that there is a threat to the patient’s life, then he must be hospitalized.
Treatment can be carried out in various ways, it all depends on its form. One can even say more, the positivity or negativity of the prognosis directly depends on the location of the arrhythmia, it could be:
- area on the atrium vault;
- atrium;
- ventricle
If arrhythmia greatly bothers the patient, then he is prescribed antiarrhythmic drugs.
Today there is no universal remedy that could cure any type of disease. Therefore, in some situations it is necessary to try several drugs until a more suitable one is found. In turn, such medications can have side effects, moreover, if they are used incorrectly, they can worsen the situation. When drug therapy does not help, and there is also a threat to life, a method such as electrical cardioversion, or as it is also called, defibrillation, is used. For a number of cases of arrhythmia treatment, pacemakers are also used, which are surgically inserted under the skin. Alternatively, radiofrequency catheter ablation is widely used.
Any of these methods will be most effective if you consult a doctor in a timely manner. Therefore, you should not neglect the health of your body and the signals it can give.
- food (615)
- products (tips) (79)
- in a hurry (62)
- from dough (53)
- national cuisine (51)
- meat dishes (49)
- vegetables (48)
- seafood (46)
- snacks (39)
- conservation (34)
- multicooker (33)
- first courses (26)
- drinks (25)
- poultry (20)
- multicooker, bread maker (19)
- festive table (19)
- diabetes (13)
- cereals (8)
- psychology (569)
- check yourself (83)
- relationships (61)
- family (56)
- mature age (56)
- emotions (51)
- experiments (47)
- stress (39)
- desire (38)
- awakening creativity (30)
- death (23)
- dream labyrinths (23)
- sorcerers, fortune tellers (16)
- loneliness (12)
- love (10)
- health (505)
- educational program (66)
- tips (61)
- first aid (49)
- diagnostics (42)
- eyes, ears, throat, nose (33)
- from the abdomen and below (29)
- useful to know (25)
- legs (24)
- head (15)
- heart, blood vessels (14)
- hands (14)
- teeth (10)
- unfamiliar about familiar (154)
- household tips (57)
- products (54)
- spices (23)
- video (147)
- house (138)
- Housing and public utilities and services (35)
- Useful tips (134)
- computer (96)
- law and rights (91)
- quotes and thoughts (83)
- predictions (68)
- Miscellaneous (67)
- among people (relationships) (65)
- Infographics (65)
- magical sounds (56)
- as we speak (55)
- about artists (55)
- design (54)
- healers (50)
- hobby (48)
- sacraments (47)
- useful links (43)
- mythology (40)
- books (40)
- My paintings and poems (36)
- parables (35)
- cinema (31)
- pension and old age (30)
- karma (27)
- children (27)
- personality (26)
- festive (23)
- note (mini) (20)
- audiobooks (20)
- (1)
- PostcardsReborn catalog of postcards for all occasions
- Weather outside the windowIn our weather it is convenient to observe: - weather phenomena for the next 5 days at 4 times of day - graphs of weather parameters such as temperature, pressure, humidity (pressure is increasing - weather at
- There are no analogues always at hand ^_^ Allows you to insert a panel with an arbitrary Html code into your profile. You can place banners, counters, etc. there
- Music player
- Download music from LiveInternet.ruSimple downloading of songs at specified URLs
Atrial fibrillation is a heart rhythm disorder in which, due to conduction disturbances, chaotic contraction of the muscle fibers of the atria occurs, but the atria as a whole do not contract, the duration of cardiac cycles fluctuates significantly and is random, excitation is not transmitted to the ventricles in a timely manner, the ventricles contract irregularly, with frequency 250-300 beats. in 1 minute, coordination between contractions of the atria and ventricles is disrupted.
Atrial fibrillation can be more or less constant or occur in attacks.
Symptoms
In some patients, atrial fibrillation may be asymptomatic. However, more often with this disease the following signs (or some of them) are observed:
Palpitations (episodes of very rapid and strong heartbeat, which is often stronger than during very intense physical activity)
Low blood pressure
Episodes of paroxysmal atrial fibrillation last from several minutes to several hours and then stop on their own.
With chronic atrial fibrillation, the heart rhythm is always irregular.
If you experience any symptoms of atrial fibrillation, get a medical examination as soon as possible. If you experience severe pain, seek emergency medical attention as it may be a symptom of a heart attack.
Causes of atrial fibrillation
In most cases, atrial fibrillation is caused by structural abnormalities and damage to the heart. But there may be other reasons:
Overactivity of the thyroid gland and various metabolic disorders
Exposure to stimulants—such as alcohol, caffeine, tobacco, medications, illicit drugs
Sick sinus syndrome (improper functioning of the sinus node)
Emphysema and other lung diseases
Previous cardiac surgery
Stress due to various reasons
The older you are, the more dangerous you are.
The older you get, the higher your risk of developing atrial fibrillation becomes.
Heart diseases. If you have a personal or family history of heart disease and/or heart surgery, your risk of atrial fibrillation increases significantly.
Alcohol abuse. Regular and excessive alcohol consumption can trigger episodes of atrial fibrillation.
Atrial fibrillation can occur with such severe heart lesions as malformations of the mitral valve (the valve between the left atrium and the ventricle), coronary heart disease, increased thyroid function (thyrotoxicosis), chronic alcoholism, and so on.
Attacks of atrial fibrillation can occur against the background of myocardial infarction, during acute poisoning with certain medications (cardiac glycosides, caffeine) or alcohol.
Sometimes an attack occurs against a background of tension and chronic stress.
The prevalence rate of atrial fibrillation is less than 1% in people under 60 years of age and more than 6% in patients over 60 years of age.
How does an attack proceed?
Attacks of atrial fibrillation can occur in different ways, it all depends on the condition of the heart.
Patients may not notice at all that their heart rhythm has changed or feel vague discomfort in the heart area.
But more often the attack is felt in the form of a sudden chaotic heartbeat. If the frequency of ventricular contraction is very high, then general weakness, dizziness, faintness, and sometimes fainting appear.
Atrial fibrillation can cause acute heart failure - the heart cannot cope with its work, which can result in pulmonary edema. The disease can also be complicated by thromboembolism (a blood clot blocks a blood vessel).
An equally common complication of atrial fibrillation is ischemic stroke - the result of insufficient blood supply to the brain.
What examinations are necessary for atrial fibrillation?
In order to establish the correct diagnosis, it is necessary to identify the atrial fibrillation itself, the conditions for its occurrence and cessation, and also to identify the disease that led to it.
To detect atrial fibrillation, you need to do an electrocardiogram (ECG), but a regular ECG does not always detect atrial fibrillation (the attack may pass). Therefore, the ECG is recorded throughout the day (this is called Holter monitoring).
Arrhythmias often occur during physical activity, so to measure the level of acceptable physical activity and evaluate the preventive effect of antiarrhythmic drugs, an ECG is sometimes done with physical activity and while taking medications.
To accurately diagnose arrhythmias, an electrophysiological study of the heart is performed with the insertion of a catheter into the heart cavity.
Medicine is prescribed only by a doctor
Arrhythmias are often treatable. Additionally, given that arrhythmia is exacerbated (or even caused) by a weak or damaged heart, you can reduce your risk of arrhythmia by living a healthy lifestyle.
Arrhythmia may have no signs or symptoms. It often happens that a doctor discovers an arrhythmia during an examination, and the patient did not suspect anything about it.
However, arrhythmia also has noticeable symptoms, for example:
Heart beats unevenly
Heart rate increases (tachycardia)
Heartbeat slows down (bradycardia)
Fainting or near fainting
These signs do not always indicate a serious problem. It happens that people who observe such symptoms do not have serious problems, but in other people life-threatening types of arrhythmias are asymptomatic.
When to see a doctor
Due to arrhythmia, you may feel like your heart is skipping beats, beating too fast or too slow.
Other symptoms may be due to the heart pumping too little blood into the blood vessels.
These are symptoms such as shortness of breath, weakness, dizziness, near fainting, and chest pain or discomfort. If you experience some of these symptoms unexpectedly or regularly, you should contact your doctor.
Risks
When the heart works irregularly, blood is poorly pumped and dispersed to the internal organs. Because of this, changes in blood pressure occur. Clots and blood clots may form. Together with the bloodstream, they enter different parts of the human body and cause a blockage in the blood supply.
Thrombus in a vessel
If a blood clot enters the blood vessels of the brain, a stroke occurs. And if a coronary vessel is blocked, the patient experiences a myocardial infarction.
If the clot enters the pulmonary artery, the person dies suddenly. Arrhythmia leads to ventricular fibrillation and can cause cardiac arrest.
To reduce the risks associated with blood pressure and extrasystole to a minimum, you need to support your heart and take certain medications.
Causes of arrhythmia
When the heartbeat rhythm fails, oxygen starvation develops, causing all tissues and organs to suffer.
Cardiac arrhythmia is a common phenomenon, often accompanied by fluctuations in blood pressure. High blood pressure can cause serious damage to the heart, brain and eyes. If there is a constant decrease in pressure, the tissues do not receive the necessary nutrition, and the cells die. The development of arrhythmia is influenced by the following factors:
- consumption of alcoholic beverages;
- smoking;
- organic myocardial damage;
- intense physical activity;
- abuse of caffeine-containing products;
- pathologies in the functioning of the central nervous system;
- unstable psyche;
- potassium deficiency in the body;
- scoliosis and other spinal diseases.
Main symptoms of arrhythmia:
Chest pain and shortness of breath are among the main symptoms of the disease.
- change in heart rate;
- feeling of interruptions, fluttering or freezing in the chest;
- fast or slow heartbeat;
- pain in the chest area;
- dyspnea;
- dizziness;
- presyncope, fainting.
Loss of consciousness is rare, only if arrhythmia develops with low blood pressure or the patient has a congenital heart defect. At the same time, sweating increases, the skin turns pale, and oxygen deficiency occurs. The clinical picture manifests itself gradually; for a long time, the pathology occurs in a latent form. During an attack of arrhythmia, you need to monitor your blood pressure. If you experience any signs of irregular heartbeat, you should consult your doctor.
Beta blockers: how to use them correctly
The point of prescribing beta blockers for arrhythmias lies in the mechanism of their action on the heart. These drugs bind to beta group receptors, through which adrenaline exerts its stimulating effects on the myocardium - it increases the frequency of contractions. By blocking the receptors with medications, this effect can be eliminated, which is important in the treatment of arrhythmia.
The most common medications in this group are Metoprolol and Bisoprolol. Compared to Amiodarone, as the standard antiarrhythmic drug, they are weaker, but in some cases they cannot be avoided. This is due to the additional effects of dilating the coronary arteries and lowering blood pressure. Therefore, any beta blockers are considered the drugs of choice for the combination of mild supraventricular and atrial fibrillation, ventricular extrasystoles with:
- hypertension;
- coronary heart disease;
- disorders of cerebral circulation.
Treatment tactics for arrhythmia when pressure changes
Patients describe arrhythmia as periodic heart palpitations followed by rapid heartbeat. Polar sensations arise. At one moment it seems that the heart is ready to burst out of the chest, and later that it may stop. In this case, the pressure that accompanies atrial fibrillation can be both low and high.
What causes frequent changes in the rhythm of heart contractions?
Diagnostics
Heart rhythm and blood pressure abnormalities can be detected at home.
Tonometers are used to measure systolic and diastolic pressure levels.
These devices are mechanical, automatic and semi-automatic. The last two options simplify the monitoring process and are able to show heart rate.
In medical institutions, echocardiograms and electrocardiograms are prescribed for diagnostic purposes.
To measure your pulse, you need to place your finger on your left wrist. It’s so easy to find out the rhythm and count the number of heartbeats.
Cardiac arrhythmia - causes Symptoms of cardiac arrhythmia
VASHE ZDOROVIE / 01.11.
The human body is structured like a well-oiled mechanism, all elements of which perform their duties in strict sequence. The computer in this mechanism is the brain, and the engine, of course, is the heart. The frequency of contraction of the heart muscle sets the pace of work of the entire body.
If the engine in a car changes speed, then this is an alarming signal, indicating that problems have arisen and in order to avoid negative consequences they need to be eliminated. The same applies to the heart - rhythm disturbances lead to undesirable consequences.
Cardiac arrhythmia - causes
In medical terminology, a heart rhythm disorder is called arrhythmia. Arrhythmia manifests itself in a violation of the heart rate, a disruption in the rhythm and sequence of contractions of organ parts. The causes of cardiac arrhythmia can be:
- alcohol abuse, smoking;
- frequent consumption of coffee;
- excessive physical activity;
- diseases of the central nervous system.
- lack of potassium in the heart, or its excess;
- diabetes mellitus, overweight person;
- metabolic disease;
- rachiocampsis;
- congenital diseases and pathologies of the heart, circulatory system, and organs of the human digestive system.
- stress, mental and emotional shock, depression.
To more accurately determine the cause of cardiac arrhythmia in each individual case, it is necessary to consult a doctor and conduct an examination of the body. And only after establishing the exact cause will the attending physician prescribe an effective course of treatment.
Cardiac arrhythmia - symptoms
Doctors say that a person cannot feel a change in heartbeat. Most likely, this statement is supported by the version that the average person simply does not know what this or that beating rhythm may indicate. Therefore, you need to know that interruptions in the functioning of the heart lead to the following symptoms of cardiac arrhythmia.
Firstly, blood pressure changes - as a rule, it decreases (see What to do with low pressure?). At the same time, the person feels weak and dizzy. His condition becomes pre-fainting, when any sudden movement or change of position leads to darkening of the eyes and pulsating beats in the temples.
Heart failure leads to a chain reaction throughout the body. Due to a failure to timely enrich the blood with oxygen, a person’s breathing is also disrupted. Shortness of breath appears, breathing becomes uneven, with freezing. Inadequate enrichment of body cells with blood leads to symptoms of cardiac arrhythmia such as noise in the head and pain in the left hypochondrium.
First aid
If an arrhythmia attack occurs, it is better to call an ambulance. Before the doctor arrives, the following measures must be taken:
- seat a person in a chair;
- loosen tight clothing;
- open the window to ensure free access of oxygen;
- measure pressure using a tonometer;
- count pulse;
- give Valocordin or Corvalol. If the attack is accompanied by a feeling of fear, it is better to use Barboval or Valerian tablets;
- if the condition remains severe, it is worth trying to normalize heart function by inducing vomiting. To do this, press on the root of the tongue. The provoked reflex often restores the heart rhythm even in the absence of vomiting.
A simple breathing exercise helps normalize heart function. You need to close your eyes and take a deep breath. Hold your breath for a couple of seconds, while pressing on your eyelids. This should be repeated three times within 10 seconds.
Correct manipulations before doctors arrive will help reduce the risk of complications to a minimum.
Often, arrhythmia develops in people who take loop diuretics (Lasix, Torasemide, Furosemide) for a long time. These drugs remove potassium from the body, which causes heart rhythm disturbances. In this case, before the ambulance arrives, it is useful to give the patient an Asparkam or Panangin tablet.
Providing first aid for cardiac arrhythmia
This disease is expressed in disturbances in the normal rhythm of the heartbeat. That is, due to a malfunction of the electrical impulses that coordinate the work of the heart, it begins to beat too quickly or too slowly. Irregularity of strokes is also observed. In addition to the heartbeat disorder, the patient experiences severe weakness, dizziness, decreased blood pressure, nausea, and fainting. Arrhythmia attacks in most cases occur suddenly and pass quickly. In such situations, medical assistance is not needed and the patient’s condition soon returns to normal. But often people suffering from this disease experience very intense attacks that require treatment and urgent measures. If a person has heart problems of this nature for the first time, then they should call an ambulance at home and take care to normalize the heartbeat before it arrives.
Urgent measures
First aid for cardiac arrhythmia, which can be provided by loved ones before the doctor arrives, is as follows:
- Providing peace. To do this, the patient with arrhythmia needs to be placed comfortably on a sofa or bed. You should try placing it lying down, and then sitting, placing a high pillow under your back. In one of these positions, a person may feel relief, because often it is changing the position of the body that helps stop the attack.
- If the patient does not feel better either in a vertical or horizontal position and the arrhythmia does not go away, then the heartbeat can be adjusted by inducing a gag reflex. They provoke it by irritating the larynx with the fingers. Even if this leads to vomiting, there is no need to panic. Such stimulation almost always helps restore the correct rhythm.
- Moral support. A sudden increase in heart rate can be frightening, and lack of air and severe dizziness often cause panic in the patient. Therefore, relatives, or people who happen to be nearby, are obliged to calm him down, explaining that everything will be fine and the attack is only temporary.
- Access to fresh air. If the attack occurs indoors, then you need to open a window or window to make it easier for the person to breathe. You can also take him outside.
- Taking a sedative. Before the patient receives qualified medical care, he should be given drugs such as Valocardin, Motherwort Tincture, Valerian, Corvalol or any other heart medicine of this group.
- Breathing therapy. During an attack of arrhythmia, it is recommended to inhale deeply, hold the air in the lungs for a few seconds and exhale smoothly. Such exercises have a beneficial effect on the functioning of the heart, bringing it back to normal.
- Manual therapy. You can close your eyes and lightly press your fingertips on your eyelids. This should be done every third second, continuing the massage for a minute.
When arrhythmia develops in the ventricles of the heart, its first sign will be a drop in pulse. That is, it will be weak and barely noticeable. In such cases, you must perform the following actions:
- Tilt the patient's head back to ensure the airway opens.
- Unfasten the top buttons on your clothes so that the collar does not squeeze your larynx.
- Monitor your heart rate.
- If the measures described above do not help alleviate the condition, then the only correct solution will be external cardiac massage and artificial respiration.
- Call emergency ambulance.
Arrhythmia can also be of atrial fibrillation in nature, and during an attack of this type of illness, first aid consists of providing the patient with rest and using sedatives. If a person experiences shortness of breath or swelling during an attack of arrhythmia, then he should be placed in a semi-sitting position, and under no circumstances should he be placed in a horizontal position. When the situation is critical and the patient’s heartbeat cannot be heard and there is no breathing, then relatives should urgently use cardiopulmonary resuscitation. The person is placed on a flat and hard surface, his head is thrown back and, positioned on his left side, artificial respiration is performed. Correctly provided first aid for cardiac arrhythmia before the doctor arrives can prevent complications of the disease and even save the lives of loved ones.
Share with friends:
Non-medicinal methods of stopping attacks
Before medicating an attack of tachycardia in young people, it is necessary to try reflex stimulation of the vagus nerve. In this case, the patient, who is in a lying position, is warned about the pain of the procedure. The method involves pressing on the eyeball, and the patient is asked to hold his breath after four breaths. While holding your breath, the doctor presses his fingers on the eyes, which should be closed.
The attack can be stopped by applying pressure to the carotid sinus. The patient is placed on his back, the doctor massages the carotid artery in the direction of the spine for several seconds. To relieve an attack, several pressures are necessary.
The Valsalva maneuver helps stop an attack of tachycardia. This is tensing the abdominal muscles while inhaling, while you need to pinch your nose and close your mouth.
The methods listed above cannot be used in cases of cerebral and coronary circulation disorders, as well as in atherosclerosis.
Treatment
Arrhythmia and blood pressure are treated with medication. Today, pharmacies offer a wide range of medications that are used to relieve heart attacks. They are produced in the form of ampoules for intramuscular or intravenous administration, or in the form of tablets.
Cardiologists prescribe the following medications to restore heart rhythm:
- Verapamil . Quickly relieves an attack of tachycardia. But in old age this remedy should be used with caution;
- Digoxin . Eliminates the causes of illness, slows down the pulse. Treatment should begin with small doses, gradually increasing the dosage;
- Quinidine . Slow-acting antiarrhythmic drug;
- Flecainide . Often prescribed by doctors to restore heart rhythm;
- Adenosine . Designed for rapid relief of arrhythmia symptoms. It works within half a minute after intravenous administration.
To prevent hypertension and heart rhythm disturbances, you can take sedatives. They improve heart function, normalize sleep, and relieve emotional tension. Among such medications, Sanosan, Persen and Antares are often used.
The drug Persen
If the goal is to relieve an attack of arrhythmia, relieve pain, and reduce the likelihood of a recurrence of an attack, then it is better to take tranquilizers. For example, Buspirone or Phenazepam. They act quickly, reduce blood pressure, normalize pulse, relieve vasospasm and reduce blood pressure.
But you need to be careful with drugs in this group. Because if taken incorrectly, they can provoke psychosis, hypertension and cardiac arrest.
Some people use decoctions of berries and medicinal plants to restore the functioning of the cardiovascular system.
For example, it is useful to drink fruit drinks and compotes from viburnum. To lower the tonometer numbers, it is recommended to brew viburnum flowers.
The fruits of chokeberry and hawthorn also give a good effect. But traditional methods are effective only in the initial stages of the disease or in combination with pharmaceutical antiarrhythmic drugs.
The effect of treatment is achieved with proper and regular use of medications. Any medication must be taken as prescribed by a doctor. Self-medication of heart problems is fraught with serious complications, including death.
Treatment and prognosis for hypertensive arrhythmia
Much depends on the type of arrhythmia, since it is one thing to prescribe therapy for sinus tachycardia, and quite another thing for fibrillation or ventricular fibrillation. Therefore, after making a diagnosis, the most appropriate method of treating hypertensive arrhythmia is selected.
Drug treatment
Since the rhythm disturbance has developed against the background of hypertension, medications are prescribed that are aimed at preventing the worsening of the underlying disease. Such drugs are considered:
- ACE inhibitors;
- statins and sartans;
- diuretics;
- beta-adrenergic receptor and calcium channel blockers;
- antiarrhythmic drugs.
The listed drugs are taken for a long time, which makes it possible to achieve a multifaceted effect on pathological processes occurring in the heart and blood vessels. Not all drugs are prescribed at once, but the most suitable combinations are selected from already proposed treatment regimens for arrhythmia in hypertension. To do this, a cardiologist is visited, who gives the necessary recommendations on taking medications.
Surgery
For arrhythmia that has developed against the background of hypertension, it is rarely prescribed. This is due to the fact that the patient, as a rule, is aged and in such cases it is unsafe to lie on the table. Also, multiple changes in the cardiovascular system associated with hypertension have become widespread, which is almost impossible to solve during one operation. Therefore, surgical intervention may be appropriate for complete blockades and some types of paroxysmal tachycardia. In other cases, drug therapy that is adequate to the patient’s condition should be selected.
Video Breathing exercises for the treatment of hypertension and arrhythmia
Ways to restore rhythm
Treatment can be carried out in various ways, it all depends on its form. One can even say more, the positivity or negativity of the prognosis directly depends on the location of the arrhythmia, it could be:
- area on the atrium vault;
- atrium;
- ventricle
If the arrhythmia greatly bothers the patient, then he is prescribed antiarrhythmic drugs. Today there is no universal remedy that could cure any type of disease. Therefore, in some situations it is necessary to try several drugs until a more suitable one is found.
In turn, such medications can have side effects, moreover, if they are used incorrectly, they can worsen the situation. When drug therapy does not help, and there is a threat to life, a method such as electrical cardioversion, or as it is also called, defibrillation, is used. For a number of cases of arrhythmia treatment, pacemakers are also used, which are surgically inserted under the skin. Alternatively, is ra widely used?
Medications
To prescribe effective treatment for arrhythmia and low blood pressure, it is necessary to find out their root cause. If the diseases are caused by pathologies of the autonomic nervous system or constant stress, then sedatives are prescribed. If the disease is organic in nature, then tranquilizers are more effective than conventional sedatives. But they are taken under the strict supervision of a doctor, in a hospital.
Attention! In total, there are three groups of drugs that are prescribed by a cardiologist to normalize heart rhythm and blood pressure.
Sedatives
The peculiarity of sedatives is that they can be used without a doctor’s prescription for preventive purposes. With the help of sedatives, blood pressure is normalized and heart rhythm is restored. Attacks of insomnia cease to bother you, and general emotional tension is relieved.
After using sedatives, nervousness is slightly reduced, without dependence or drowsiness.
Sedatives have a combined composition. Among the components: bromides, herbal medicinal preparations and barbiturates. As already noted, the most popular sedatives for low blood pressure and heart rhythm disturbances are motherwort and valerian.
These sedatives are used for preventive purposes to relieve emotional stress. To do this, motherwort is taken 30-50 drops with 50 ml of plain water. It is undesirable to take such drugs if a person does not experience obvious discomfort.
Tranquilizers
If a person is intolerant to antiarrhythmic drugs, then treatment is carried out using tranquilizers. They are used to restore heart rhythm. Tranquilizers differ from sedatives in that they lower blood pressure and reduce heart rate during tachycardia.
The use and dosage of tranquilizers is only as prescribed by the attending physician. Among the drugs used are Diazepam, Elenium and Phenazepam. If pathological changes in the heart cause a rhythm disturbance, then, in addition to relieving the arrhythmia, you need to treat the underlying disease. A competent doctor, as a rule, will be able to reduce the dosage while still leaving the therapy effective.
Antiarrhythmic
A group of these drugs are used to normalize heart rhythm. In this case, antiarrhythmic drugs will not be prescribed if the patient needs to relieve pain or reduce the likelihood of recurrence of arrhythmia. With the help of antiarrhythmic drugs, the conductivity of the heart muscle is improved and metabolic processes are restored.
Typically, the following antiarrhythmic drugs are prescribed:
- Aymalin.
- Ethacizin.
- Pulse norm.
- Novocainamide.
- Quinidine.
- Rhythmonorm.
In this case, the attending physician selects the drug and dosage, assessing the severity of the disease. All instructions and prescriptions of the cardiologist or arrhythmologist must be followed in full. To maintain effectiveness, do not stop taking it prematurely or reduce the dose. Because in this case the risk of relapse increases.