Causes
Torsade de pointes, characterized by a prolonged QT interval, may be congenital or acquired as a result of the action of drugs. Genetic variants include:
- hereditary syndromes that may be accompanied by deafness;
- gene pathology - today scientists have discovered six more hereditary defects associated with prolongation of the PQ interval. These genes encode transmembrane K and/or Na channels.
Hereditary factors are rare; more often the occurrence of pathology is influenced by the use of drugs. These include:
- antiarrhythmic medications;
- phenothiazines, butyrophenones;
- antifungal drugs;
- antihistamines;
- some are antiviral;
- antibiotics, especially macrolides;
- antidepressants;
- organophosphorus compounds (OPS);
- cocaine.
Provoking factors may be poor nutrition or starvation, alcoholism, endocrine and cardiovascular diseases, subarachnoid hemorrhage. Existing genetic pathologies, congenital heart defects, and concomitant somatic defects can cause an attack. The most common causes are listed above, but each case should be considered individually by your doctor.
Treatment of this type of arrhythmia
Torsade de pointes tachycardia is a serious disease that should be treated by a qualified specialist.
Important
! Since this type of tachycardia often occurs after taking medications, it is imperative to inform your doctor about the use of any medications.
Treatment of the disease is divided into urgent and permanent. When attacks of pathology occur, immediate resuscitation assistance is necessary. In the event of a sharp drop in blood pressure, cardioversion is used, and medications to stop the attack are also administered, such as magnesium sulfate, adrenergic blockers, lidocaine, which shortens the intervals.
In cases where the appearance is associated with taking medications, their use is immediately stopped and additional treatment is prescribed to remove harmful substances from the body. When diagnosing a stable torsade de pointes arrhythmia with altered areas in the ventricles of the heart, patients are indicated for surgical intervention. For this purpose, an automatic defibrillator-cardioverter is implanted.
As a permanent treatment, antiarrhythmic drugs are prescribed under the strict supervision of a doctor and ECG monitoring; prescriptions are also possible (“Nerviplex-N”, “Ascorutin”, “Napravit”, etc.).
In addition to drug therapy, it is very important for the patient to adhere to the correct lifestyle, it is advisable not to overwork, both physically and mentally, and to avoid nervous strain. Proper nutrition also plays an important role; experts recommend:
- do not eat fried, spicy or salty foods;
- do not abuse flour, sweets and coffee;
- give up alcohol;
- use lean meat, dairy products, cereals for cooking;
- eat vegetables and fruits;
- drink about 2 liters of water per day.
Pathophysiology: mechanism of occurrence of disorders
Ari develops by prolonging the repolarization phase. The electrocardiogram, in addition to prolongation of the QT interval, shows the presence of noticeable U waves at rest. These ECG changes reflect prolonged repolarization with the development of early subsequent depolarization.
Pathology can lead to hemorrhages into the ventricular tissue, causing myocardial infarction.
Repolarization occurs in the myocardium when the number of positive ions (mainly potassium) exceeds the number of sodium and calcium ions, the concentration of which should decrease. Potassium channel dysfunction causes intracellular excess positive charge, which delays ventricular repolarization. This state of the myocardium leads to the emergence of a specific type of recurrent arrhythmic tachycardia.
Causes, symptoms and treatments for ventricular tachycardia
How is this disease diagnosed?
The presence of the disease can be determined by carrying out simple procedures. When a person complains to a doctor about certain ailments, he is sent for an examination of possible ECG signs. Using a special device, the heart rhythm is measured. The cardiogram will immediately show whether there is tachycardia or not.
In rare cases, such an examination does not reveal pathology. To be completely sure, experts advise undergoing an ultrasound, which shows the functioning of the heart as a whole. At this stage, you can detect areas in which ari appears class=”aligncenter” width=”500″ height=”375″[/img]
How do doctors fight the disease?
It is not uncommon for doctors to prescribe antiarrhythmic medications. In other cases, long-term treatment with removal of the cardioverter-defibrillator. And, for example, tachycardia with paroxysms (pirouettes) dictates mandatory outpatient treatment.
Treatment of ventricular tachycardia of the unsustained pirouette type may not be considered an emergency option. Only if the attacks lengthened did the frequency of the organ beat increase. Then the doctor prescribes an antiarrhythmic drug.
The main responsibility of the attending physician is to prevent the death of the patient. The second most important is the elimination of arrhythmia. Implantation of a cardioverter-defibrillator is the optimal solution in serious situations.
Long-term treatment is inappropriate if the disease appears as a result of a recent myocardial infarction. In other cases, patients require hospitalization.
What complications are possible?
- An acute form of decreased blood circulation in the brain followed by loss of consciousness with silent ventricular tachycardia. This complication often plunges the patient into a prolonged coma.
- Heart failure with characteristic pulmonary edema. If the disease is not treated in a timely manner, the complication will become regular and even fatal.
- Stopping blood circulation. The optimal solution here is to restart the organ using defibrillation and implantation of a pacemaker.
What preventive measures should be followed?
To prevent illness, it is worth considering some particularly important recommendations.
So, a person with a tendency to such a disease needs to worry less, avoid mental illness and excessive physical activity.
Ventricular tachycardia requires proper nutrition - excluding fatty foods, giving up any alcohol and cigarettes, reducing coffee consumption. Medical advice: frequent walks in the fresh air, fruits and vegetables in your daily diet.
Symptoms
Patients often complain of fainting. Loss of consciousness is explained by the fact that the heart contracts at a frequency of 200-250 beats per minute and does not provide sufficient blood supply to the brain. Patients who remain conscious experience a strong heartbeat. There may also be chest pain and a feeling of shortness of breath. Sometimes QT prolongation is diagnosed after rhythm has been restored. You should immediately call an ambulance, and perform indirect cardiac massage until the doctors arrive.
If you want to know everything about tachycardia, we recommend watching the video below at the link. Causes, symptoms, diagnosis and signs that it’s time to see a doctor - talk about all this in 7 minutes. Enjoy watching!
Symptoms of tachycardia type pirouette
The early stage of the pathology may be asymptomatic. Subsequently, signs of pathology begin to appear against the background of a lack of oxygen in the heart muscle, which occurs with an increase in attacks.
With torsades de pointes, the number of ventricular contractions per minute increases sharply, so the movement of blood through the vessels (hemodynamics) is sharply disrupted. Most patients lose consciousness in this case, but attacks occur periodically. When consciousness is preserved, a person feels a palpitation, which should not be normal. During an attack, pathology may manifest itself with other signs:
- severe dizziness;
- frequent rhythmic pulse (weak filling);
- low blood pressure.
The danger of torsade de pointes is primarily that it can lead to gastric fibrillation. This complication carries a risk of death.
During attacks, the heart rate changes, sometimes increasing and sometimes decreasing. In the absence of complications, the indicators normalize on their own.
Diagnostics
The diagnosis is made on the basis of an ECG. The wavy peaks of the QRS complexes are clearly visible on the film. The complexes themselves change their orientation around the isoline. An increased QT interval is present on the electrocardiogram outside of an attack. Normally, its value is within 0.44 s. You should pay attention to family history: if one of your relatives has an increased interval, then the risk of developing torsade de pointes increases.
- Example of tachycardia associated with digoxin toxicity
Such tachycardia often does not last long and goes away on its own, but sometimes leads to hemodynamic destabilization with subsequent collapse. It can also develop into ventricular fibrillation. In this case, immediate assistance will be required: indirect cardiac massage and stimulation of myocardial activity with an electric current discharge.
- Torsade de pointes resulting from hypokalemia
The ECG of a patient with hypokalemia is shown in the photo below: the patient experienced a brief self-terminating paroxysm of torsade de pointes with an “R on T” layering effect.
- Torsades de Pointes
Treatment methods
Complex treatment of arrhythmia is not always required, and it will depend directly on the diagnosis. It is required in cases where the risks of complications are very high or if the symptoms of the disease are too pronounced. Since treatment is divided by type of tachycardia, in each case it has a number of features.
In case of a slow heartbeat, the cause of the problem is addressed, only in the most severe cases resorting to the implantation of a pacemaker.
Treatment for rapid heartbeat is usually carried out according to one of the following schemes:
- Drug therapy. Help restore normal rhythm and control heart rate. If atrial fibrillation is present, blood thinners are also used to avoid the formation of blood clots. Any use of antiarrhythmic drugs is carried out only under the supervision of a physician.
- Catheter ablation. With this effect, a special catheter is implanted into the cavity of one of the vessels leading to the heart. At the end of it there are electrodes that begin to produce radio waves, heat or cold. The result of such actions is damage (ablation) to the area of cardiac tissue that provoked the arrhythmia.
- Maneuvers related to the vagus nerve. Treatment of a certain type of tachycardia that begins in the atria is carried out using special exercises. They include periodic relaxation and straining, coughing, and washing with cold water. Vagal techniques for normalizing heartbeat and blood pressure levels often show their effectiveness in the initial development of tachycardia, but they are effective only for a few of their types.
- Cardioversion is performed only if the patient has certain indications, as well as when tachycardia is combined with fibrillation. With electric shock pacing, a shock penetrates the heart muscle through devices located on the chest. Treatment is also carried out with drug cardioversion. The impulses or substances sent help restore the normal beating rhythm.
Clinical case
A 56-year-old patient called the emergency medical team.
Complaints: headache and chest discomfort. This state lasts several hours before the call. There is a history of hypertension, but the patient does not undergo regular treatment. Sometimes, when blood pressure rises above 200/120, she takes Captopril at a dose of 25-50 mg. Before the complaints arose, I consumed about 1 liter of wine. According to him, he periodically abuses alcoholic beverages. At the time of inspection, productive contact is available. Skin, breathing, abdomen - without any features. Cardiac activity is rhythmic, tones are muffled. BP 160/90, heart rate=Ps 90 per minute. The abdomen is soft and painless. The “tapping” symptom is negative on both sides. Physiological functions are normal. The patient's ECG is presented below:
During the recording of the tape, the patient stated that she began to feel very bad and dizzy. The ECG shows pirouette tachycardia, which immediately turned into large-wave atrial fibrillation.
The patient's condition is extremely serious: clinical death was diagnosed. Pulse and pressure are not determined. Our team immediately moved the patient to a hard surface (floor) with resuscitation measures: mechanical ventilation, chest compressions, administration of Atropine, Adrenaline, magnesia; Two defibrillations were performed. Peripheral vein catheterization and hospitalization to the cardiac intensive care unit are provided directly, bypassing the emergency room. At the time of admission to the hospital, the patient was conscious and had no complaints. BP 130/90, heart rate=Ps 90 beats per minute. Breathing on your own.
Causes
Torsades de pointes is provoked by many factors. It can be caused by excessive stress and stress or severe heart pathologies. Most often, rhythm disturbance occurs under the influence of:
- Stress. In such situations, adrenaline is released in the body, which leads to an increase in heart rate.
- Abuse of energy drinks, tea, coffee.
- Insufficient amount of fluid in the body. The heart begins to pump blood faster, thus trying to compensate for the lack of oxygen and nutrients.
- Overeating. The heart rate increases because more blood is concentrated in the digestive tract.
- Physical activity. Enhanced metabolic processes in muscles require sufficient oxygen and nutrients.
If the influence of these factors is eliminated, the heart function returns to normal. But this only works in the case of healthy people.
The development of tachycardia of the pirouette type is observed when there is not enough magnesium and potassium in the blood.
This form of heartbeat is characterized by the fact that during contraction the myocardium touches the left ventricle and causes insufficient oxygen supply to the atrium. A simultaneous but incorrect contraction occurs, since the pulse is very high - up to 350 beats.
As a result, a pathology of synchronicity of cardiac muscle functions develops, and the contractility of the ventricles decreases. This is dangerous due to the sudden stop of the organ.
The development of this type of arrhythmia occurs under the influence of mental disorders such as vagotonia. It is caused by lack of sleep, constant stress, smoking, drinking alcohol and coffee in large quantities.
Rhythm disturbances are provoked by medications such as cardiac glycosides, tranquilizers, and antidepressants.
The risk of developing the problem increases with a hereditary predisposition.
Treatment
As already discussed in the example above, an acute attack is accompanied by immediate hemodynamic disturbances and quickly progresses to clinical death. It is eliminated by unsynchronized cardioversion, starting from 100 J. But a repeated attack occurs almost instantly, so slow intravenous administration of 2 g of magnesium sulfate is necessary. If these measures do not help, then you need to repeat the bolus (rapid) injection of magnesium into a vein after 5-10 minutes. You can also use lidocaine for drug-induced tachycardia of the “pirouette” type. Remember that antiarrhythmics of classes I, II and III are prohibited.
Modern evidence-based medicine makes recommendations for reducing the QT interval and changes in the processes of repolarization and depolarization. Such protocols are confirmed experimentally by clinical trials.
To restore rhythm, drugs are used:
- Magnesium sulfate.
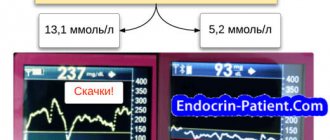
Magnesia is the drug of choice for pirouette-type tachycardia. Recommended even if the plasma magnesium level is initially sufficient. The medicine in a dose of 2 g for adults and 25-50 mg/kg for children is administered intravenously over one to two minutes in case of a sudden attack leading to life-threatening hemodynamic disturbances. In vitro studies have shown that magnesium reduces the amplitude of early depolarization to subthreshold levels by blocking calcium in the body. Therefore, the administration of the drug should be accompanied by correction of hypokalemia to a serum K concentration of more than 4.5 mmol/l. An intravenous infusion of a polarizing mixture containing magnesium and potassium is used.
- β-blockers
Esmolol is a cardioselective β-blocker, administered intravenously. The peculiarity of the drug is that it acts quickly and quickly leaves the body. Propranolol has similar properties, but its effect is more persistent and does not disappear in a short time. Therefore, Esmolol is more often used in clinical practice.
- Lidocaine
Lidocaine is a sodium channel blocker. Loading dose – 2 mg/kg, then administered as needed. The drug is believed to indirectly suppress the development of arrhythmia by reducing the duration of the action potential. However, studies show the success of the drug in only 50% of reported cases.
Ventricular arrhythmias
Often encountered in clinical practice, patients require careful evaluation to determine the individual prognosis of these arrhythmias and the possible risk of ventricular fibrillation (VF) and sudden cardiac death. Frequent ventricular arrhythmias include: ventricular extrasystole (VC); ventricular tachycardia (VT); ventricular fibrillation (VF); accelerated idioventricular rhythm.
Ventricular extrasystole
Ventricular extrasystole (VC) is a premature excitation of the heart that occurs under the influence of impulses emanating from various parts of the ventricular conduction system. Single monomorphic PVCs can arise as a result of both the formation of re-entry of the excitation wave (re-entry) and the functioning of the post-depolarization mechanism. Repeated ectopic activity in the form of several successive PVCs is usually due to the re-entry mechanism. The source of PVCs in most cases are the branches of the His bundle and Purkinje fibers. With PVCs, the sequence of repolarization changes, a displacement of the RS-T segment above or below the isoline, and the formation of an asymmetric negative or positive T wave are observed. The RS-T displacement and the polarity of the T wave are discordant to the main wave of the ventricular complex, directed in the direction opposite to this wave.
An important sign of PVCs is the absence of a P wave before the extrasystolic QRS complex, as well as the presence of a complete compensatory pause. With PVCs, there is usually no “discharge” of the SA node, since the ectopic impulse arising in the ventricles cannot retrogradely pass through the AV node and reach the atria and SA node. In this case, the next sinus impulse unimpededly excites the atria, passes through the AV node, but in most cases cannot cause another depolarization of the ventricles, since after the PVC they are still in a state of refractory. With left ventricular ES, there is an increase in the interval of internal deviation in the right chest leads V1, V2 (more than 0.03 s), and with right ventricular ES - in the left chest leads V5, V6 (more than 0.05 s).
To assess the prognostic significance of PVCs, V. Lown and M. Wolf (1971) proposed a grading system. Based on the results of 24-hour Holter ECG monitoring, 6 classes of PVCs are distinguished: class 0—absence of PVCs within 24 hours of monitoring; Class 1 – less than 30 PVCs are recorded during any hour of monitoring; Class 2 - more than 30 PVCs are recorded in any hour of monitoring; Class 3 - polymorphic PVCs are registered; class 4a - monomorphic paired PVCs; class 46 - polymorphic paired PVCs; Class 5 - 3 or more PVCs in a row are recorded within no more than 30 seconds. Grades 2–5 PVCs are associated with a greater risk of ventricular fibrillation (VF) and sudden cardiac death.
In 65-70% of healthy people, individual, monomorphic isolated PVCs are recorded, belonging to class 1 according to the classification of V. Lown and M. Wolf, and are not accompanied by clinical and echocardiographic signs of organic heart pathology. Therefore, they are called “functional PVCs.” Functional PVCs are recorded in patients with hormonal imbalances, cervical osteochondrosis, NCD, when using aminophylline, glucocorticoids, antidepressants, diuretics, and vagotonics.
In individuals with increased activity of the parasympathetic system, PVCs disappear during physical activity.
Organic PVCs are characterized by a serious prognosis and occur in patients with ischemic heart disease, myocardial infarction, post-infarction cardiosclerosis, hypertension, heart defects, myocardial infarction, myocarditis, pericarditis, dilated cardiomyopathy, hypertensive cardiomyopathy, and chronic heart failure. More often, polytopic, polymorphic, paired VT and even short episodes (“jogging”) of unstable VT are recorded. The presence of “organic” extrasystole does not exclude a certain role of neurohormonal disorders in the occurrence of arrhythmia. Patients who have been identified as having organic PVCs undergo: a biochemical blood test (K+, Mg2+ and other parameters); 24-hour Holter ECG monitoring; EchoCG with determination of EF, diastolic dysfunction; study of heart rate variability. These studies make it possible to identify the possible risk of VF and sudden cardiac death and determine treatment tactics for patients.
Ventricular tachycardia
Ventricular tachycardia (VT) is a sudden onset and just as suddenly ending attack of increased ventricular contractions up to 150-180 beats. (less often - more than 200 beats or within 100-120 beats per minute), usually while maintaining the correct regular heart rhythm). Mechanisms of VT paroxysms: re-entry of the excitation wave (re-entry), localized in the conduction system or working ventricular myocardium; ectopic focus of increased automaticity; ectopic focus of trigger activity.
In most cases, in adults, VTs develop according to the reentry mechanism and are reciprocal. Reciprocal VTs are characterized by a sudden acute onset immediately after the VT inducing the onset of the attack. Focal automatic VTs are not induced by extrasystoles and often develop against the background of increased heart rate caused by physical activity and an increase in catecholamine levels. Triggered VTs also occur after a PVC or an increase in heart rate. Automatic and triggered VT is characterized by tachycardia with a gradual achievement of the rhythm frequency, at which stable VT remains.
There are streets with cardiac pathology (acute MI, post-infarction aneurysm, DCM, HCM, arrhythmogenic dysplasia of the pancreas, heart defects, MVP, digitalis intoxication). In 85% of cases, VT develops in patients with coronary artery disease, and in men 2 times more often than in women. ECG signs: 1. A sudden onset and just as suddenly ending attack of increased heart rate up to 140-150 beats per minute (less often - more than 200 or within 100-120 beats per minute) while maintaining the correct rhythm. 2. Deformation and expansion of the QRS complex more than 0.12 due to its discordant location of the RS-T segment and the T wave. 3. The presence of AV dissociation - complete separation of the rapid rhythm of the ventricles (ARB complexes) and the normal sinus rhythm of the atrium (P waves).
Differential diagnosis of VT and supraventricular AT with wide QRS complexes is of paramount importance, since the treatment of these two rhythm disturbances is based on different principles, and the prognosis of VT is much more serious than that of supraventricular AT. A reliable sign of a particular form of AT is the presence of VT or the absence of AV dissociation with periodic “captures” of the ventricles. This in most cases requires intracardiac or transesophageal recording of ECG P waves. However, even with a routine clinical examination of a patient with paroxysmal tachycardia, by examining the veins of the neck and auscultation of the heart, it is possible to identify signs characteristic of each type of PT. In supraventricular tachycardia with AV conduction 1:1, the frequency of the arterial and venous pulses coincides. Moreover, the pulsation of the neck veins is of the same type and has the character of a negative venous pulse, and the volume of the first tone remains the same in different cardiac cycles. Only in the atrial form of supraventricular AT is there an occasional loss of arterial pulse associated with transient second-degree AV block.
Figure 30.
Ventricular tachycardia
(M.L. Kachkovsky)
There are three clinical variants of VT: 1. Paroxysmal unsustained VT is characterized by the appearance of three or more consecutive ectopic QRS complexes, recorded during an ECG monitor recording within no more than 30 s. Such paroxysms increase the risk of VF and sudden cardiac death. 2. Paroxysmal sustained VT, lasting more than 30 s. It is characterized by a high risk of sudden cardiac death and significant changes in hemodynamics. 3. Chronic or continuously recurrent VT - long-term repeated relatively short tachycardic “jogs”, which are separated from each other by one or more sinus complexes. This variant of VT increases the risk of sudden cardiac death and leads to a gradual increase in hemodynamic disturbances.
Polymorphic ventricular tachycardia "pirouette"
A special form of paroxysmal VT is polymorphic VT (torsade de pointes), which is characterized by an unstable, constantly changing shape of the QRS complex and develops against the background of an extended QT interval. It is believed that the basis of bidirectional spindle-shaped VT is a significant prolongation of the QT interval, which is accompanied by a slowdown and asynchronism of the repolarization process in the ventricular myocardium, which creates the conditions for the occurrence of reentry of the excitation wave (reentry) or the appearance of foci of transient activity. In some cases, bidirectional VT may develop against the background of a normal QT interval.
The most characteristic feature of VT of the “pirouette” type is a constant change in the amplitude and polarity of ventricular tachycardia complexes: positive QRS complexes can quickly transform into negative ones and vice versa. This type of VT is caused by the existence of at least two independent but interacting reentry circles or several foci of trigger activity. There are congenital and acquired forms of VT of the “pirouette” type.
The morphological substrate of this VT is inherited - long QT syndrome, which in some cases (with an autosomal recessive type of inheritance) is combined with congenital deafness. The acquired form is much more common than the hereditary form. Develops against the background of an extended QT interval and pronounced asynchrony of ventricular repolarization.
ECG signs of VT: 1. The ventricular rate is 150-250 per minute, the rhythm is irregular with fluctuations in RR intervals within 0.2-0.3 s. 2. QRS complexes of large amplitude, their duration exceeds 0.12 s. 3. The amplitude and polarity of the ventricular complexes changes over a short period of time. 4. In cases where P waves are recorded on the ECG, separation of the atrial and ventricular rhythm (AV dissociation) can be observed. 5. Paroxysm of VT usually lasts several seconds, stopping spontaneously, but there is a pronounced tendency for repeated recurrence of attacks. 6. Attacks of VT are provoked by PVCs. 7. Outside of an attack of VT, a significant prolongation of the QT interval is recorded on the ECG. Since the duration of each attack of pirouette-type VT is short, the diagnosis is often made based on the results of Holter monitoring and assessment of the duration of the QT interval in the interictal period.
Figure 31.
Ventricular tachycardia type "pirouette"
(M.A. Kachkovsky)
Ventricular flutter and fibrillation
Ventricular flutter (VF) is a frequent (200-300 per minute) and rhythmic excitation and contraction. Ventricular fibrillation (flicker) is an equally frequent (200-500 per minute), but chaotic, irregular excitation and contraction of individual muscle fibers, leading to the cessation of ventricular systole (ventricular asystole). Main ECG signs: 1. With ventricular flutter - frequent (200-300 per minute), regular and identical in shape and amplitude flutter waves, reminiscent of a sinusoidal curve. 2. With ventricular fibrillation (flicker) - frequent (200-500 per minute), but irregular random waves, differing from each other in different shapes and amplitudes.
The main mechanism of VT is the rapid and rhythmic circular movement of the excitation wave along the ventricular myocardium (re-entry) along the perimeter of the infarcted zone or area of the LV aneurysm. VF is based on the occurrence of multiple random micro-re-entry waves formed as a result of pronounced electrical inhomogeneity of the ventricular myocardium.
The causes of TG and VF are severe organic lesions of the ventricular myocardium (acute myocardial infarction, chronic ischemic heart disease, post-infarction cardiosclerosis, hypertensive heart, myocarditis, cardiomyopathies, aortic heart defects).
Figure 32.
Ventricular flutter
(M.A. Kachkovsky)
There are primary and secondary VF. Primary fibrillation is associated with acutely developing electrical instability of the myocardium in patients who do not have fatal circulatory disorders, severe heart failure, or cardiogenic shock. The causes of primary VF may be acute coronary insufficiency (MI, unstable angina), myocardial reperfusion after effective revascularization of the heart muscle, or surgical manipulation of the heart.
Primary VF is in most cases successfully treated with electrical cardioversion, although patients subsequently remain at high risk of VF relapses. Secondary VF is a mechanism of death in patients with severe organic pathology: cardiogenic shock, CHF, post-infarction cardiosclerosis, dilated cardiomyopathy, and heart defects. Secondary VF is usually very difficult to treat and in most cases ends in the death of the patient.
Polymorphic ventricular tachycardia with prolongation of the QT interval (pirouette type)
polymorphic ventricular tachycardia with prolongation of the QT interval (pirouette type)
Ventricular tachycardia of the “pirouette” type is associated with an increase in the duration of repolarization of cardiomyocytes, determined on the ECG by a prolongation of the QT interval (congenital or acquired), and its immediate triggering factor is a slowdown in heart rate, which leads to a sharp prolongation of the interval.
The diagnostic criteria are the following ECG signs (Fig. 58):
1) cyclical changes in the direction of the QT complex vector in the range of 180 ° with an average frequency of 10-15 complexes
2) the connection between the occurrence of ventricular tachycardia and a decrease in heart rate. Ventricular tachycardia is often preceded by severe sinus bradycardia and complete atrioventricular block.
3) prolongation of the Q-T interval in sinus rhythm complexes immediately preceding ventricular tachycardia.
The ventricular rhythm frequency during paroxysm of ventricular tachycardia of the “pirouette” type ranges from 150-250 per minute.
Clinical picture and course . Most attacks end spontaneously and are asymptomatic or accompanied by dizziness and temporary loss of consciousness. However, in such patients the risk of transformation of ventricular tachycardia into ventricular fibrillation and sudden death is significantly increased.
Treatment and secondary prevention . The method of choice is temporary electron pacing, preferably atrial, with a heart rate of 90-100 per minute, which allows reducing the duration of the QT interval. Class IV antiarrhythmic drugs lidocaine and mexiletine have the same ability. Even in the absence of hypomagnesemia, iatrogenic ventricular tachycardia of the “pirouette” type can be suppressed by the administration of magnesium sulfate in a dose of 2-3 g, which is associated with the elimination of trigger activity due to blockade of calcium channels. Intravenous administration of potassium salts also has a good effect. In the case of a prolonged attack, they resort to electrical defibrillation, which, however, gives an unstable effect.
To prevent relapse of polymorphic ventricular tachycardia, o. Subsequently, the use of other drugs known to prolong the QT interval should be avoided. It is also important to prevent the development of hypokalemia and hypomagnesemia.
We also recommend that you take a look
Follow-up therapy and prevention
Subsequent therapy is aimed at preventing the recurrence of ventricular fibrillation. After all, the result can be fatal without timely help. International heart health organizations recommend regular use of β-blockers. The effectiveness of their use is 68–90%. Sodium channel blockers, such as Meksitylen, also have a good effect.
If syncope persists during β-blocker therapy, implantation of a pacemaker-defibrillator is indicated. It must be remembered that this operation does not mean the abolition of drug treatment.
The main advice to patients and their relatives is to know the list of drugs that prolong the QT interval and avoid taking them.
The last resort treatment is left-sided sympathectomy at the level of the cervicothoracic spine.
Prevention
To prevent the development of this type of tachycardia, there are certain rules that must be followed to avoid manifestations of the disease:
- Maintain proper diet.
- Avoid eating flour and sweets, fatty foods, and strong coffee.
- Include more vegetables and fruits in your diet.
- Stop drinking alcohol and tobacco.
- Engage in feasible sports.
- Spend time outdoors regularly.
- Do not take medications without a doctor's prescription.
- Treat concomitant pathologies.
- Refrain from stress and mental fatigue.
To avoid the manifestations of the disease, since it poses a considerable danger to human life, it is recommended to visit a doctor on time. When a disease is detected, you must strictly follow all instructions that will help overcome the disease.
It got its name because of the pattern of the cardiogram, which shows a frequent and wave-like amplitude of the QRS complexes. An attack of this type of arrhythmia is difficult to predict. It may end abruptly or cause ventricular fibrillation.
Polymorphic
Ventricular tachycardia with a changing QRS morphology or electrical axis is classified as polymorphic. Ventricular tachycardia of the pirouette type on the ECG has the following meanings:
- The rhythm may be irregular. Polymorphic is usually very fast (100-320 beats per minute) and unstable. There are several types of polymorphic ventricular tachycardia. The most common cause is myocardial ischemia. The second most common cause is a long QTc interval (Long QT syndrome).
- Familial catecholaminergic polymorphic ventricular tachycardia (CPVT) is an inherited disorder in which emotional or physical stress causes an arrhythmia, which can lead to circulation and cardiac arrest. This type can be bidirectional. Diagnosis is made by stress testing because sympathetic activity causes tachycardia.
- Brugada syndrome causes polymorphic VT (mainly during sleep or fever).
Early repolarization and hypertrophic obstructive cardiomyopathy also lead to polymorphic VT.
Bidirectional ventricular tachycardia on the ECG, a photo of which is attached, means that the QRS morphology alternates from one beat to the next. In most cases, it repeats between two variants of the QRS complex. Seen in familial CPVT, digoxin excess, and long QT syndrome.
Prevention and prognosis
The main preventive measures are the following:
The prognosis of this disease is unfavorable. At the first occurrence of complaints and timely contact with a cardiologist, the prognosis can be improved, since effective therapy will be prescribed in a timely manner.
If you neglect your body’s “cry for help,” polymorphic pirouette tachycardia can turn into ventricular fibrillation and be fatal.
It is extremely important to tell the doctor all the details of the course of the disease: the time and frequency of symptoms, medications taken, and the presence of similar manifestations in close relatives.
No matter how serious the disease, you can always improve your quality of life if you seek help in a timely manner. Torsade de pointes arrhythmia often requires only ECG monitoring and an integrated approach to treatment to be confirmed. The outcome and prognosis, if basic rules are followed, can have a favorable course.
This term is used to describe one of the forms of ventricular tachycardia, which is called torsades de pointes or torsades de pointes.