Low leukocytes in the blood - what does this mean?
Relative leukopenia occurs more often when the balance of different types of leukocytes is disturbed: the percentage of some types decreases due to an increase in others.
Clinicians identify the following reasons:
- Autoimmune diseases. When the immune system functions abnormally, a reverse reaction occurs - the immune system destroys the cells of its own body, allowing pathogens to pass through - provocateurs of the inflammatory process. Such diseases include systemic lupus erythematosus, rheumatoid arthritis, and scleroderma.
- Thyroid diseases. Failure in the functioning of the endocrine system contributes to a decrease in leukocytes. In case of persistent leukopenia, it is necessary to conduct an examination for diabetes mellitus, hypothyroidism, and parahyperthyroidism.
- Drug treatment. Long-term use of certain medications causes a decrease in white blood cells. Among the drugs are barbiturates, antiparkinsonian antibacterial agents, sulfonamides, antispasmodics. Symptoms of toxic effects of drugs are nausea, vomiting, thinning and discoloration of stools.
- Decreased levels of vitamin B. Impaired synthesis of vitamin B in the child’s body leads to disruption of the formation of new white blood cells. Prevention of vitamin deficiency in children includes diet correction and the introduction of synthetic vitamin complexes.
- Kostman's disease. Congenital pathology, which consists of a persistent decrease in all blood components from the group of leukocytes along with the simultaneous growth of other cells that perform immune function. Kostman syndrome is characterized by chronic infections of the skin, mucous membranes, and internal organs. The prognosis is unfavorable.
- Cyclic neutropenia. The disease is accompanied by exacerbations and remissions, characterized by a decrease in neutrophils and a decrease in the immune response. Against the background of pathology, the body copes poorly with its protective function and is susceptible to frequent respiratory or intestinal infections.
Hereditary factors, oncology, and HIV can provoke the development of persistent leukopenia. The pathological condition is often secondary in nature - it becomes a consequence of the underlying disease. When diagnosing a persistent decrease in leukocytes, an extensive examination is carried out.
Reasons for the development of pathology in children
The reasons for the progression of leukopenia in young patients are divided into two groups:
- Infectious:
- sepsis;
- sixth and seventh types of herpes;
- typhus, paratyphoid;
- flu;
- brucellosis;
- rubella;
- measles;
- AIDS and HIV;
- Non-infectious:
- leukemia;
- plasmacytoma;
- ion irradiation;
- diffuse connective tissue pathologies;
- autoimmune diseases;
- anaphylaxis;
- hypersplenism;
- Addison-Beermer anemia;
- metastasis of neoplasms to the bone marrow;
- autoimmune diseases;
- endocrine pathologies (hypothyroidism, diabetes).
The development of leukopenia in newborns can be provoked by intrauterine inflammatory processes.
Normal indicators
The level of leukocytes in the blood of infants and preschool children is slightly higher than the physiological norm in adults due to the imperfection of the immune system. There are the following indicators of normal leukocyte levels in children by age:
- newborn babies – 10-30×109 l;
- from 1 to 6 months – 8-21×109 l;
- from 1 to 2 years – 7–15×109 l;
- 3–4 years – 5–12×109 l;
- 5–7 years – 5–10×109 l.
Be sure to take into account the concentration of other types of white blood cells. The norm must correspond to the age of the child and fall within the reference values.
Deciphering involves assessing the concentration of all blood cells in accordance with the child’s age, his life and clinical history. Venous blood is suitable for analysis. The study is carried out on an empty stomach.
If you receive a result with a low level of leukocytes, you should retake the blood after 2-4 weeks. Be sure to evaluate the blood composition comprehensively. Additionally, urine and feces are collected for differential diagnosis.
Symptoms
The main signs and symptoms of leukopenia (neutropenia) in children are determined by the form of the disease and the severity of the painful period.
The following clinical picture is formed:
- The child’s immune system decreases progressively. This occurs due to infectious actions occurring in the child’s body. This may be pneumonia, periodontitis, stomatitis, pharyngitis, gingivitis, hemorrhagic vasculitis.
- The development process in children slows down.
- The infectious nature of the disease is very difficult and can become complicated.
Infectious skin lesions
Agranulocytosis is an extreme degree of leukopenia. There are two types: immune and myelotoxic.
Immune occurs after drug poisoning. Progresses sharply. It begins with an elevated temperature and the rapid development of infectious respiratory diseases.
Myelotoxic agranulocytosis occurs at one moment, in the absence of an appropriate prerequisite. The level of white cells, platelets, and reticulocytes in the blood decreases sharply. The main symptom is an increase in body temperature. The cellular composition of the blood undergoes great changes. The bone marrow is significantly affected.
Post-infectious leukopenia manifests itself in the post-influenza period. This procedure occurs briefly. After recovery, the blood test returns to normal.
How to increase?
True leukopenia is the field of study of a hematologist, pediatrician, neurologist, infectious disease specialist and geneticist. Based on the analysis data and other studies obtained, tactics for managing the child are prescribed. Complicated leukopenia requires drug therapy. The treatment regimen consists of prescribing the following drugs:
- recombinant drugs based on interferon;
- interleukins to stimulate the immune system;
- colony-stimulating agents for autoimmune diseases;
- plant-based immunostimulating drugs for long-term use.
The main treatment depends on the root cause of the pathological process. If the cause is hypothyroidism, hormone replacement therapy with drugs based on levothyroxine sodium is required; if diabetes mellitus, sugar-controlling drugs are prescribed.
If the HIV status is positive, lifelong antiretroviral therapy is prescribed. The blood test is repeated during treatment to assess the dynamics of the child’s condition. With long-term adequate treatment, the viral load on the body decreases, and the child’s immune status is restored.
Inflammatory and infectious complications require antibiotic therapy. A low white blood cell count may be transient. In this case, the composition of the blood is restored after the underlying cause is eliminated.
Treatment at home
Regardless of the causes of leukopenia, non-traditional treatment methods are auxiliary. Popular ways to increase the level of leukocytes in the blood are:
- Decoction of rose hips. A handful of rosehips are washed, poured with 2 liters of water and boiled over low heat for 30–45 minutes. Afterwards, the composition is allowed to brew and cool under natural conditions. The healing decoction is filtered, a little honey is added to improve the taste and the child is given 300-500 ml during the day.
- A mixture of aloe and honey. Aloe leaves are washed, cut into small pieces and crushed with a blender or meat grinder until mushy. The composition is mixed with honey to taste and taken 1-2 tbsp. spoons after meals.
A positive result is observed with long-term use of a decoction based on ginseng, eleutherococcus, chamomile, and peppermint. Some components may provoke allergic reactions in children.
Complications of leukopenia
A persistent decrease in white blood cells disrupts the balance of other blood constituents and also leads to a number of the following complications:
- iron deficiency anemia against the background of a simultaneous decrease in hemoglobin and erythropoietin;
- thrombocytopenia and internal bleeding (when platelets are sharply reduced);
- acute inflammation of the mucous membranes, skin;
- infections of internal organs.
With leukopenia, treatment of any infectious diseases is long-term. Life-threatening pathogens with a decrease in white blood cells are staphylococci, gonococci, streptococci, Pseudomonas aeruginosa and Escherichia coli. A severe complication of leukopenia in children is sepsis.
Low leukocytes in a child’s blood require mandatory correction to avoid complications. Prevention of leukopenia consists of observing a protective regime, timely and correct treatment of infectious diseases, an age-appropriate diet, and an active lifestyle.
Pathogenetic mechanisms
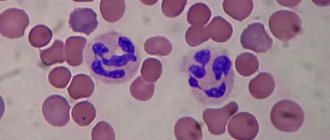
- White bodies are classified as follows: they are divided into agranulocytes in the blood and granulocytes. Agranulocytes are divided into lymphocytes and monocytes, granulocytes - basophils, eosinophils, neutrophils.
- The white cell mechanism is disrupted. Leukocyte growth experiences various pathological influences. In this regard, there are many reasons that cause the decline in the formation of white blood cells.
- The second is severe damage to leukocytes. This variant of leukopenia occurs very rarely. Anti-leukocyte antibodies in the blood destroy white cells. The destruction of white bodies is also caused by large ranges of radiation.
- The mechanism of redistribution leukopenia, which occurs as a result of stressful conditions, physical exertion on muscles, due to stagnation of leukocytes. In this case, white cells do not leave the blood completely and remain in the vessels of the muscles, lungs, and kidneys.
- Another pathogenetic mechanism of leukopenia in a child is too much loss of mesh tissue. Occurs with burns of large areas of the body, suppuration, and disruption of the integrity of the lymphatic vessels.
- Blood thinning. This is a rare type of disease. It is a consequence of infusion therapy.
Photo of leukocyte
The child has low leukocytes in the blood
Children's blood test results are very important, as they allow us to assess whether the child is healthy or has any disease that requires medical attention. One of the most important indicators is the number of leukocytes. Depending on various pathologies and external factors, this amount may vary. In what cases are leukocytes determined to be below normal and is this dangerous for the child’s health?
What quantity is considered reduced?
Leukocytes are white blood cells that protect the body from various unfavorable factors, such as infections. Their number may change during the day, after physical activity, changes in temperature, food intake and other factors. In this case, the lower limit of the norm in a child is considered to be:
In a newborn
At 1 month
At 1 year
At 5 years old
At the age of 15
Leukopenia is diagnosed when the indicator decreases by more than 2 x 10 9 / l from the age norm.
Causes of leukopenia
A decrease in the number of white blood cells is due to:
- Lack of substances that are required to form such blood cells. These substances include B vitamins, ascorbic acid, iron, zinc, selenium, proteins, iodine and many other compounds. If their intake is insufficient, the child will also have a decrease in the number of red blood cells and the amount of hemoglobin.
- Destruction of white blood cells , which can be caused by bacterial infections, medications, toxins and many other factors.
- Immune response to a viral infection , in which leukocytes move to tissues affected by the virus, and there are fewer of them in the bloodstream, although the overall number of leukocytes in the body does not decrease.
- Bone marrow dysfunction. The production of leukocytes in it can be inhibited by certain genetic diseases, tumor processes, poisons, ionizing radiation, chemotherapy and autoimmune processes.
We recommend watching an educational video that highlights the problem of low white blood cell levels in children:
- For viral infections, such as chickenpox, mononucleosis or rubella. A reduced rate in such diseases is noted for some time after recovery.
- With hypovitaminosis, as well as with insufficient nutrition (starvation).
- For low blood pressure.
- For aplastic anemia.
- For purulent infections and septic lesions.
- In the last stages of tumors , as well as in acute leukemia .
- For systemic diseases. Leukopenia is observed in rheumatoid arthritis, as well as in lupus.
- After treatment with cytostatic drugs, which are most often prescribed for tumors. Also, a decrease in white blood cells is provoked by the use of steroids, antibiotics, anti-inflammatory, anticonvulsants and some other drugs.
- After exposure to radiation. Such rays inhibit the production of leukocytes, so their decrease will occur during radiotherapy or radiation sickness.
- In case of severe allergies (anaphylactic shock).
- For endocrine diseases, for example, with lesions of the thyroid gland (hypothyroidism) or diabetes.
- With hyperfunction of the spleen , as a result of which blood cells are destroyed in greater numbers.
Prevention
Preventive measures are aimed at eliminating those factors that provoke leukopenia.
- To avoid drug-induced neutropenia, doses of medications taken should be reduced to avoid severe forms of the disease.
- To improve the immune status, introduce more proteins, fresh vegetables, fruits, and herbs into the children's menu. At the same time, limit carbohydrates.
- To form the rules of a healthy lifestyle in children. Accustom to compliance with hygiene rules and feasible physical activity.
- Monitor blood counts regularly. Treat diseases in a timely manner.
Patients who have undergone treatment are monitored at the dispensary, with periodic blood leukogram monitoring.
We also know from the school biology curriculum that blood consists of plasma, red blood cells, platelets and leukocytes. Each of these components plays a special, very important role for the human body. For example, leukocytes. These are colorless (more often called white) blood cells, the main purpose of which is to protect the body from adverse effects such as viruses, infections, etc. It is leukocytes that provide people with immunity to all sorts of ailments. To find out the level of leukocytes, it is necessary to do a laboratory blood test. The functional state and number of leukocytes shows the state of a person’s health – good, fair or poor.