This pregnancy 3. Childbirth 3. 1st child is alive and well, 2nd child died on the first day of life.
The woman suffers from type 1 diabetes mellitus (insulin dependent). Sent with a preliminary conclusion We take 31-32 weeks of fetal edema.
An ultrasound examination reveals 1 live female fetus in the uterine cavity, in a cephalic presentation. Fetometry data corresponds to: 30 weeks (based on the size of the head and limbs) (size of the abdomen at 35 weeks due to hepatosplenomegaly, increased perinephric tissue), fetal weight 2110 g +/- 300 g. (95 percentile 1850 gr). There is thickening of the subcutaneous fatty tissue in the head (double contour) and extremities, especially the thighs. The characteristic face of the fetus: puffy, round, with pronounced cheeks. Polyhydramnios.
Conclusion: We take 30 weeks Diabetic fetopathy: macrosomia, hepatosplenomegaly, increased subcutaneous fat layer and perinephric tissue. Polyhydramnios.
Diabetes and pregnancy
The diagnosis of diabetes mellitus occurs quite often in people of different ages. Moreover, in many cases, people live with high blood sugar levels, without even suspecting that they have such a dangerous disease or a predisposition to it. Diabetes mellitus is dangerous due to its complications that can lead to coma and even death. Women suffering from this disease or on the verge of diabetes mellitus should pay special attention not only to pregnancy, but even to planning it. With diabetes, a woman who wants to become pregnant must achieve stable remission of the disease. This must be done so that the child does not suffer from such a pathology as diabetic fetopathy.
Labor activity
Often during pregnancy, the expectant mother experiences hypoglycemia. Low sugar levels lead to decreased labor. It takes a lot of glucose to contract the uterus. If there is a lack of energy, childbirth will be very difficult, complications are possible. Losing consciousness is not uncommon. In severe cases, coma is possible.
Hypoglycemia can be treated using various methods:
- drink sweet water, for the preparation of which you will need to add 2 tablespoons to a glass of water,
- 500 ml of glucose 5% is administered intravenously,
- up to 200 mg of hydrocortisone is administered,
- no more than 1 ml of adrenaline.
Performing such procedures can significantly facilitate childbirth, and thereby reduce the risk to the child’s life.
Embryofetopathies
Newborn babies may suffer from pathologies that develop during fetal development. They are called fetopathies. Such pathologies, or diseases, are divided into two main groups, determined by the factors that caused them:
- exogenous - external;
- endogenous - internal.
In both cases, the child appears with health and development problems that can affect his subsequent life. Diabetic fetopathy of the fetus is an endogenous problem, as it is caused by diabetes or prediabetes of the mother.
general characteristics
An endocrine disease associated with constant fluctuations in glucose levels is identified by a high risk of fetal fetopathy. In diabetes, this is associated with destabilization of internal organs, such as the kidneys or liver. Identification of embryofetopathy is a guide to performing a cesarean section.
The favorable completion of the process is influenced by factors such as the type of disease, the presence or absence of complications, and restorative tactics. The specifics of managing the condition and the stage of compensation are taken into account. In general, premature control is a guarantee of bearing a child, and its absence threatens sudden birth.
Causes of the disease
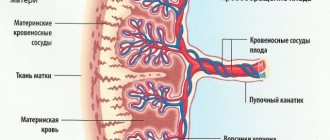
Diabetic fetopathy is a pathological disease of newborns that develops as a result of diabetes mellitus or a pre-diabetic condition of a pregnant woman. Why does diabetes have such an impact on the unborn baby? With diabetes, a person has elevated blood sugar levels, which has a very bad effect on the organs and tissues of the whole body. In this case, the kidneys, nervous system, vision, blood vessels, muscular system, and genitourinary organs are affected. Sugar easily penetrates the placental barrier into the baby’s blood, which means that the child’s body is subject to the same disorders that adults suffer from diabetes. Until 4 months of pregnancy, the fetus does not yet have the ability to produce insulin, since the pancreas has not yet formed, which means that the child simply “chokes” on blood glucose. When the pancreas is formed and begins to work, it is not easy for it; it immediately begins to work for wear and tear, which leads to hypertrophy of this organ. The level of insulin in the blood of the fetus increases, and this leads to another problem - macrosomia: the organs of the unborn child become larger than necessary, and the respiratory system suffers. The adrenal glands and pituitary gland begin to suffer. All this can lead to fetal death; according to some data, about 12% of fetal mortality occurs due to uncompensated maternal diabetes.
If a newborn child is diagnosed with “diabetic fetopathy”, treatment must begin from the very first days of his life, because in the vast majority of cases (90%) the baby of a woman with diabetes is born with various intrauterine disorders.
Signs, symptoms
- macrosomia (large fetus weighing more than 4 kg)
- characteristic appearance (disproportionate size, when the volume of the abdomen exceeds the size of the head by more than 2 weeks, short arms and legs, swollen face, broad shoulders, large belly)
- incidence of malformations
- excess deposition of subcutaneous fat
- swelling of the soft tissues of the fetus
- delivery time has been shortened
- high perinatal mortality
- intrauterine developmental delay
- breathing disorder
- decreased activity
- cardiomegaly (enlargement of the liver, kidneys and adrenal glands, but they are poorly developed)
Also, the circumference of the baby’s head can be significantly smaller than the circumference of the shoulder girdle. This leads to numerous postpartum injuries, since the baby’s head is relatively small and there are no difficulties in removing it, but the removal of the shoulders is very difficult.
Therefore, at first they can free one hand, even to the detriment of the baby (they can seriously injure it). They have overly developed subcutaneous fat, there may be edema, and they often have hypertrichosis.
But the most striking indicator of fetal fetopathy is macrosomia.
Most practicing doctors are inclined to believe that the main reason for the formation of malformations is hypoglycemia and hypoinsulinemia in the early stages of pregnancy; additional unfavorable factors are hypoxia, vascular disorders, and lipid metabolism disorders.
What does a baby with diabetic fetopathy look like?
Pregnant women should undergo regular medical examinations. This is done, among other things, to avoid embryonic fetopathies. Elevated blood sugar levels, even in a woman who is not diagnosed with diabetes mellitus and does not suffer from such a pathology as elevated glucose levels before pregnancy, serves as a signal that the development of the fetus may not be as successful as we would like. Therefore, both doctors and the expectant mother need to take urgent measures to preserve the baby’s health. Diabetic fetopathy of the fetus has the following symptoms:
- the child is very large: the body weight of the newborn is more than 4 kilograms;
- bluish tint of the newborn’s skin as a result of oxygen starvation;
- small red rash - petechial hemorrhages;
- severe swelling of the face, body, limbs;
- large belly due to a thick layer of subcutaneous fat;
- the baby’s body lubrication is quite abundant and looks like fatty cottage cheese;
- Due to insufficient liver function, the development of so-called newborn jaundice is possible - the baby’s skin and the sclera (whites) of the eyes acquire a yellow tint.
Diabetic fetopathy of newborns has clear signs of a health problem.
Diagnosis of a pregnant woman
For a pregnant woman, regular observations by a gynecologist managing her pregnancy are indicated. He conducts an examination and prescribes the necessary examinations and tests. But not only the pregnancy itself should be observed by a specialist. A woman who plans to become a mother should take this step wisely, and contacting a doctor for an examination is the beginning of planning for motherhood. Diabetic fetopathy of newborns is a serious problem for the unborn child; it is dangerous not only for his health, but also for his life. Diabetes mellitus of the expectant mother or a predisposition to this disease should be treated with special medications that will help reduce blood glucose levels. A pregnant woman should regularly check her sugar level in order to reduce it, although antiglycemic drugs do not penetrate the placental barrier and will not help a fetus affected by excess maternal blood sugar.
A predisposition to diabetes mellitus (prediabetes) requires the same intervention from a doctor as the disease itself. Pregnancy changes the entire body of a woman and its functioning. Careful monitoring and assistance if necessary is the basis of the work of a doctor managing a pregnancy. An expectant mother must undergo regular blood sugar tests. Ultrasound examinations, routinely carried out in the 10-14th week of pregnancy, will reveal emerging pathologies - a large fetus with disturbed body proportions, an enlargement of the fetal liver and spleen according to the results of examination, an excessively large amount of amniotic fluid.
Prenatal treatment
Every woman undergoes routine examinations and tests during pregnancy. If there is a suspicion of abnormalities, the doctor prescribes additional comprehensive diagnostics. The results obtained are compared. If the diagnosis is confirmed, treatment must be started immediately. This will prevent harmful effects on the embryo.
With this diagnosis, sugar levels and blood pressure readings are constantly monitored. If necessary, additional therapy using insulin is prescribed. It is very important that the diet is balanced. It should contain a sufficient amount of vitamins necessary for the normal development of the fetus. In other cases, the doctor prescribes a vitamin complex. In this position, a woman is advised to adhere to a diet and exclude fatty foods. The daily diet should not exceed 3000 kcal. Before giving birth, foods that contain large amounts of easily digestible carbohydrates are added to the diet.
Based on the results of the ultrasound and constant monitoring, the doctor determines the appropriate time for childbirth. If the pregnancy proceeds without deviations, then the best option would be 37-38 weeks. If there is a threat, the deadlines are shifted. This is done in order to reduce the risk to the child.
During treatment, nutritional adjustments are made
Diagnosis of a newborn
Not only the external signs of diabetic fetopathy are characteristic of a newborn child suffering due to elevated maternal blood sugar levels. He has a lot of functional problems. A newborn child with diabetic fetopathy has poor respiratory system functioning. A special substance - surfactant - helps the lungs expand when the baby takes his first breath. It is formed in the lungs of the fetus immediately before birth and, at the moment of the first breath, “unfolds” the alveoli so that the child can breathe. If the lungs are immature, as happens with diabetic fetopathy, then they have a deficiency of surfactant, which leads to breathing problems. If timely measures are not taken (administration of special medications, connection to a special life support system), the death of the newborn may occur. In addition to respiratory failure, immediately after birth a child diagnosed with diabetic fetopathy experiences changes in blood tests such as increased hemoglobin levels and an increase in red blood cells (polycytonemia). Sugar levels, on the contrary, are lowered, since the hypertrophied pancreas produces a huge amount of insulin.
How to treat
If a pregnant woman suffers from diabetes or has a predisposition to it (so-called prediabetes), then the child will most likely receive a diagnosis of “diabetic fetopathy.” Clinical recommendations are aimed at stimulating the organs and systems of the newborn that were damaged during intrauterine development. Since blood sugar levels are low, the baby is given a certain amount of glucose in the first two hours of life and applied to the mother’s breast every two hours to replenish nutrients and immunomodulatory substances. Replenishing the newborn's blood glucose levels is necessary, since he can no longer obtain it through the mother's blood. Hypoglycemic coma and death of the baby can occur. It is necessary to carry out respiratory stimulation by introducing special surfactant preparations and connecting the newborn to the ventilation system. Diabetic fetopathy is dangerous due to insufficient amounts of potassium and magnesium, which are involved in neurological functions, so the newborn is given medications containing these microelements. If the child has jaundice, he is placed in an incubator with ultraviolet irradiation, covering his eyes with a special opaque bandage.
Necessary tests taken from the baby after birth
- glycemic level is determined
It is monitored immediately after birth, and then a blood sample is taken for glucose after 1, 4, 8, 12, 20, 24 hours. The analysis is repeated on the day of discharge.
- biochemical blood test for calcium and magnesium
Blood serum is determined 6, 24 and 48 hours after birth.
- blood biochemistry
The concentration of protein and its fractions, urea, the level of potassium, sodium, cholesterol, and, if necessary, also determine: alkaline phosphatase, AST, ALT, etc.
- general blood analysis
Hematocrit must be determined
- general urine analysis
On the first and third days of the baby’s life.
- electrocardiography
It is performed if there is a suspicion of possible heart defects.
Complications of the disease
Despite all the measures taken, diabetic fetopathy in newborns has the most unpredictable consequences. Perhaps the child will stabilize, gradually all organs and systems will begin to function within normal limits, and the baby will develop and grow well. But there are often cases when all the measures taken by doctors after the birth of such a baby do not lead to positive results, and the child dies. But in the vast majority of cases, a child with diabetic fetopathy develops the following complications:
- respiratory distress syndrome of newborns - impaired respiratory function with hypoxia of tissues and organs;
- neonatal diabetes mellitus;
- acute heart failure as a result of hypoxia and/or hypoglycemia.
If measures are not taken in time to stabilize the condition of a newborn with diabetic fetopathy, then the child’s well-being may deteriorate and pathologies may develop that can lead to disability and death.
Examination plan for a child from a mother with diabetes mellitus
Helps prevent the development of life-threatening complications.
Includes:
- Inspection and assessment of physical parameters (weighing and measuring height).
- Complete blood count, determination of hemoglobin and hematocrit.
- Tracks heart rate and breathing.
- Blood gas assessment (helps identify respiratory disorders at an early stage).
- Biochemistry: bilirubin, electrolytes.
- Monitor blood glucose every two hours from birth.
- Ultrasound of the heart and abdominal organs.
- If respiratory disorders develop, a chest x-ray is indicated.
Examination of a newborn from a mother with diabetes is always carried out urgently! For this purpose, the child is transferred to a specialized department.
Monitor for little ones
Prevention of diabetic fetopathy
Diabetes mellitus can develop in a woman planning a pregnancy, regardless of her health status, because it is a very insidious disease that does not make itself felt for a long time. But pregnancy must be approached responsibly, and when planning to become a mother, a woman should visit a doctor and undergo a diagnostic examination. A diagnosis of diabetes mellitus or a pre-diabetic condition is not a reason to give up motherhood. You just need to take measures in advance that can lower your blood sugar levels to acceptable levels and maintain them throughout your pregnancy. This must be done in order to protect the child from such a serious health problem as diabetic fetopathy.
The recommendations of the doctor who will manage the pregnancy must be strictly followed. A schedule of visits to the antenatal clinic, routine blood and urine tests, and ultrasound will allow timely identification of emerging abnormalities in the intrauterine development of the fetus and take measures to stabilize the condition of the unborn baby. A woman who suffers from high blood sugar should know that drugs that lower it in the mother’s body do not penetrate the placental barrier into the child’s body, which means that this indicator must always be maintained at normal levels with the help of medications and diet.
Mother and child together against diabetes
Fetal diabetic fetopathy is a disease that develops during the fetal development of the baby and directly depends on the mother’s body. That is why a woman should take responsibility for her health when she is just thinking about becoming a mother. You shouldn’t rely on chance when you are going to give life to a little man, he must be as healthy as possible, because too many dangers await the nascent life in addition to the poor health of the mother. A timely examination and quality measures to reduce the threat to the well-being of the fetus will allow a woman to bear and give birth to a healthy child. Observations suggest that a newborn child diagnosed with diabetic phenopathy, with attentive and competent treatment and care, by the age of 2-3 months can almost completely overcome existing problems. Yes, some symptoms of this disease will remain, but basically the child will be able to lead a full life.