This condition may indicate the presence of a serious pathology of the digestive tract. Each case of bleeding should alert not only the patient, but also the doctor. To make a diagnosis, it is necessary to undergo a complete examination of the body. Minor blood loss can later lead to serious complications and cost the patient his life.
There may be causes of bleeding from the anus that are not significant, but are characterized by serious diseases of the digestive system. Over time, the disease can become chronic and its symptoms become more frequent and more severe.
Bleeding can come from different parts of the digestive organs; the higher the organ is located, the darker the blood will be. When the source of bleeding is the lower gastrointestinal tract, then the blood discharge from the anus will be bright red.
When to call an ambulance?
There are several factors when you need to immediately call an ambulance if you are bleeding from the anus:
- When the bleeding is intense and does not stop for a long time;
- If the bleeding is accompanied by vomiting mixed with blood;
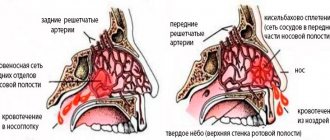
- During bleeding there is discharge from the nose, with the formation of bruises and hematomas;
- When, during bleeding, the patient experiences severe weakness and deterioration in general condition;
- Along with bleeding, the patient's temperature rises and severe abdominal pain appears.
How dangerous is bleeding during illness?
Recurrent bleeding from the anus in proctology is considered a dangerous symptom. It indicates a breakthrough of the vessels of the large intestine and requires urgent hemostatic therapy. Constant blood loss causes serious harm to the health of a sick person.
Important! It has been established that daily blood loss of 50-100 ml is not restored by the body and leads to chronic iron deficiency anemia.
A decrease in the level of red blood cells and hemoglobin is accompanied by a cessation of oxygen supply to tissues and organs. The brain and myocardium are the first to suffer. The state of oxygen deficiency (hypoxia) gradually disrupts the functions of the body. Blood pressure drops, dizziness, weakness, and palpitations appear.
A sharp decrease in immunity makes it possible for the infection to easily penetrate into the nodes and spread to surrounding tissues. Therefore, against the background of anemia, patients with hemorrhoids are much more often susceptible to complications (paraproctitis, the formation of fistulas, cracks in the rectum). The infection becomes severe and causes general sepsis.
Acute bleeding accompanies thrombosis of the node with necrosis and rupture of the wall. A condition arises that is dangerous to human life.
Causes of bleeding
Causes of bleeding from the anus:
- Erosive gastritis and duodenal ulcer;
- For cirrhosis of the liver and thrombophlebitis of the veins of the spleen and esophagus; Signs of liver cirrhosis in men can be found here.
- Various oncological formations;
- Intestinal tuberculosis;
- Intestinal polyps;
- Ulcerative colitis of a nonspecific nature;
- Crohn's disease;
- Anal fissures;
- Varying degrees of hemorrhoids;
- Dysentery;
- Typhoid fever;
- Hemorrhagic fever;
- Helminthic infestations that can affect and injure the intestines;
- Venereal diseases of the genital organs;
- Salmonellosis;
- Enteroviruses.
Blood diseases:
- Leukemia;
- Mesenteric thrombosis.
Blood diseases
In diseases of the bone marrow and peripheral blood, clinical analysis shows intense anemia, a decrease in nominal cells and platelets. There are tumor cells in the bone marrow fluid.
For blood diseases, all symptoms are divided into several categories:
- All symptoms characteristic of anemia;
- Frequent fungal, colds and bacterial diseases, which also indicate a decrease in immunity;
- Acute platelet shortage. This indicates frequent nosebleeds, bruises and hematomas for no reason.
The cause of blood disease is the replacement of healthy blood cells with blast cells. These parasitic cells do not perform the necessary functions for the blood. To stop the process of replacing healthy cells with diseased ones, it is necessary to take cytostatics. If heavy bleeding is observed, the patient is transfused with red blood cells or other blood substitutes.
What are false bleedings?
The appearance of clots in feces may be a false manifestation, which is caused by the consumption of certain dishes and foods. Therefore, if you notice changes in the color of feces, you should not immediately start sounding the alarm. First, remember what foods you consumed, because it is possible that this was the main reason for the change in stool color.
If after a few days the clinical picture does not change, then you need to visit a doctor, since blood discharge in the feces is always an unfavorable sign. Before visiting a proctologist, you can conduct a self-diagnosis, but it should not replace a professional examination.
Self-diagnosis methods
Using self-diagnosis, of course, you won’t be able to find out about the possible cause, but it will help you collect information about your condition, which will simplify the diagnosis in the future.
If you detect blood clots in your stool, pay attention to the following factors:
- the color of the blood and its amount;
- the presence of clots and blood streaks;
- the place of the greatest concentration of blood - inside or outside the feces;
- presence of blood on underwear or on toilet paper.
These symptoms will allow you to make an accurate diagnosis.
Visit to the proctologist
To establish the exact root causes of blood formation during bowel movements, it is necessary to conduct a thorough diagnosis and visit a specialist - a proctologist. Typically, a complete examination consists of several stages. The most effective examination methods:
- palpation of the rectum is a mandatory procedure for making a diagnosis;
- general tests - blood, urine and feces;
- taking anamnesis;
- additional research, if necessary.
Sometimes a procedure such as an ultrasound of the abdominal area and rectum may be prescribed. The latter is not a very pleasant procedure, but with its help you can exclude or, conversely, confirm the presence of tumors, oncological formations and other serious diagnoses.
What to do if there is bleeding from the anus during bowel movements?
When you notice a slight admixture of blood in the stool, you need to contact a proctologist, who will prescribe you to undergo an examination and determine the cause of the bleeding. If the bleeding is intense and accompanied by poor health, then you need to call an ambulance.
There are several types of examinations that will help determine the nature of bleeding:
- The patient is prescribed to undergo sigmoidoscopy. This will help examine the lower intestines. As a result, hemorrhoids, anal fissure and neoplasms in the rectum and sigmoid colon can be identified;
- Colonoscopy . Deeper examination of the large intestine;
- Irrigoscopy. It is carried out by introducing a contrast agent and x-ray into the intestines;
- Fibrogastroduadenoscopy. An endoscope is used to examine the stomach and duodenum. During the study, a piece of tissue may be taken from the patient for a biopsy;
- Laparoscopy. This is a joint diagnostic and therapeutic procedure. This will allow you to completely examine the abdominal cavity and take fluid for a biopsy;
- Fecal occult blood test. It is very common that there is no bleeding, but there is an admixture of blood in the stool. If blood is detected in the analysis, then it is necessary to undergo the above examination. Treatment for bleeding from the anus depends only on the identified cause. And these may not always be serious pathologies, but it is simply necessary to see a doctor and get diagnosed.
Possible ailments
Advanced infectious diseases, especially chickenpox and salmonellosis, are fraught with heavy blood loss. In this case, the asymptomatic incubation period can last up to 18 hours. During this time, the infection manages to affect the intestinal walls. As a result, every second patient experiences liquefied stools and releases up to 50 ml of blood per day.
Possible causes of the disease can also be:
- helminthic infestation;
- nonspecific ulcerative colitis, accompanied by mushy stools with cherry-colored blood clots;
- Crohn's disease, which promotes dysfunction of several parts of the intestine;
- the third stage of rectal cancer, when the tumor affects neighboring organs and lymph nodes.
Benign formations include polyps. According to statistics, they are found in 35% of patients suffering from rectal bleeding. With proper treatment, a quick recovery is possible in 95% of cases.
Haemorrhoids
Already at the second stage of the disease, increasing pain during bowel movements is possible. In the third stage, hemorrhoidal seals increase in size and become inflamed from time to time. Internal lumps tend to thin the rectum, thereby preventing proper bowel movements. Anal fissures, hardened feces, prolonged diarrhea and large nodules can cause bleeding.
In this case, the daily volume of blood released in different patients is 45–90 ml. In the latter case, the hemoglobin level decreases to critical levels, and the body is no longer able to cope with destructive processes on its own. If the disease is neglected, daily blood loss will exceed 180–220 ml. This can trigger the development of severe anemia.
Heavy bleeding is observed in the case of necrosis of hemorrhoidal seals. If you do not see a doctor in time, death is possible.
Anal fissures
We are talking about small and deep ruptures, accompanied by pain after almost every bowel movement. And since a lot of small capillaries are concentrated in the rectum, the cause of rectal bleeding can be:
- toilet paper made from cheap recycled materials containing lead;
- abuse of hamburgers, cheese (50%), sushi, potato and rice dishes - such food compacts feces and creates a feeling of incomplete bowel movement;
- long hours of labor;
- engaging in anal sex is fraught with exacerbation of paraproctitis, in which blood flows out with pus;
- exacerbation of chronic hemorrhoids and rectal prolapse, which is dangerous when the outer and longitudinal layers of the rectum come out.
Intestinal polyps
Small polyps the size of a pea do not pose a threat to the life of patients. Large ones often reach the size of a tennis ball and cause rectal bleeding in 68% of cases. Along with the clots, mucus is released from the anus. The result of this phenomenon is often a deterioration in the absorption of nutrients and the accumulation of toxins in the body.
Scarlet drops on paper are the main sign of polyps. Considering that people suffering from hemorrhoids also experience similar phenomena, it is important to consult a doctor as soon as possible. Perhaps this is not a manifestation of polyps at all, but a harbinger of colorectal cancer.
Sometimes benign formations prevent complete bowel movement. This leads to prolonged constipation and squeezing pain in the abdomen.
Oncology
In some cases, rectal bleeding is caused by cancer of the rectum and sigmoid colon. When the tumor completely disintegrates, a sick person releases up to 80 ml of blood per day. In case of damage to a large vessel - over 90 ml. The main symptoms of colorectal cancer are sticky blood in the stool, anorexia and almost 25 percent weight loss.
Improper treatment of the disease is fraught with serious disturbances in the functioning of the intestines. This means:
- poisoning of the body with undigested food particles and decay products;
- weakened synthesis of immune system cells;
- impaired intestinal motility;
- insufficient production of vitamins and hormones;
- the body's inability to suppress viral attacks.
Diverticulosis
The main cause of the disease is the abuse of fatty foods, physical inactivity and recent intestinal infections. Long-term constipation increases pressure in the digestive organs, resulting in the formation of diverticula. These are bulging areas where fecal matter accumulates.
As the disease worsens, the likelihood of scarlet rectal bleeding increases. Abundant release of connective tissue - up to 75 ml per day - contributes to nagging pain in the abdomen. But intestinal obstruction with impaired secretion of gastric juice is much more dangerous. Since the body's cells are susceptible to any structural changes, dysfunction of all organ systems is possible.
Other diagnoses
With ulcerative colitis, most large vessels are affected, so bleeding occurs in different places. At the initial stage of the disease, clots are released in minimal quantities, and pain is possible only in 35% of cases. When colitis worsens, stool resembles foamy red liquid. Not everyone can survive in such conditions.
Crohn's disease is rarely accompanied by heavy bleeding from the anus. However, almost 45% of patients develop anemia as a result of connective tissue leakage. In this case, large vessels are damaged.
In some cases, acute intestinal infections contribute to rectal bleeding. At the same time, women and men secrete up to 55 ml of blood daily, and children – up to 20 ml. By coming into prolonged contact with digestive enzymes, the blood irritates the intestinal walls. This causes foul-smelling stools stained with red liquid.
Haemorrhoids
Hemorrhoids are accompanied by bleeding as a result of the expansion of hemorrhoids and their prolapse from the intestine. Bleeding usually occurs after bowel movements. When the blood does not completely leave the passage, it later appears in the stool in the form of clots. Also, mucous discharge from hemorrhoid cones leads to itching.
Manifestations
Hemorrhoids and bleeding occur in various pathologies:
- With constipation, childbirth and heavy lifting, pressure in the abdominal cavity is observed;
- Sedentary lifestyle and little movement;
- With stagnation of blood in the pelvis;
- Alcoholic drinks and spicy foods.
Treatment
Treatment for hemorrhoids can be conservative or surgical. Nowadays, there are many effective and modern methods of treating this disease.
Conservative treatment is as follows:
To begin with, the patient is prescribed the use of rectal suppositories. The drug contains hemostatic components to quickly stop bleeding, painkillers and anti-inflammatory drugs.- It is also necessary to take a special diet during treatment. The food should contain fiber; it is this that relieves the patient from constipation, which leads to the development of hemorrhoids. It is not recommended to consume spicy food and alcoholic drinks.
- You can use Zdorov cream wax. Price and instructions are described here.
The surgical treatment method is based on:
- The patient undergoes electrocoagulation of the hemorrhagic node , after which the tissue on it dies and falls off;
- Sclerotherapy is based on the introduction of a special agent into the node, which leads to the collapse of its walls. This technique can eliminate hemorrhoids of the first and third degree;
- Latex ligation. A ring is put on the base of the hemorrhagic node, as a result of which the node does not receive nutrition, and the blood supply to it is disrupted, and the tissue in it dies; During the surgical procedure, the surgeon excises nodes and lumps, and the wound is stitched.
How to stop
People suffering from hemorrhoids and anal fissures need to know what to do if there is bleeding from the anus. To stop bleeding, use ice. Cold instantly affects the walls of blood vessels and narrows the capillaries. If bleeding occurs against the background of hemorrhoids, then a cold compress will help relieve the pain.
There are several ways to stop bleeding with ice:
- Using an ice compress or lotion. This method is effective for external hemorrhoids. The bandage is folded into 4 layers, soaked in ice water and, taking a position lying on your side, applied to the anus for 5 minutes. You can wrap ice cubes in a bandage. For this purpose, decoctions of medicinal herbs (oak bark, chamomile), which have an anti-inflammatory and drying effect, are frozen.
- Use of ice suppositories. They are used if there are internal bleeding hemorrhoids. Small cone-shaped containers are made from thick paper and water or herbal decoctions are poured into them. Place in the freezer until hardened. Before use, remove the paper, dip the candle in warm water, and then carefully insert it into the anus for 5 seconds.
- Using the Krinus device. It replaces ice suppositories and compresses for hemorrhoids, and prevents the effects of cold on the skin and internal organs.
If a person has pathologies of the kidneys, pancreas and bladder, then the use of cold is contraindicated for him: low temperatures can cause the development of inflammatory processes. In this case, it is better to use hemostatic drugs:
- Detralex;
- Dicynone;
- Vikasol.
The use of these drugs has contraindications and side effects, so their long-term use must be discussed with a doctor.
If bleeding occurs in adults, it is recommended to use a hemostatic collagen sponge 6-9 mm thick, which can be purchased at a pharmacy. The porous sponge is impregnated with boric acid and furatsilin and is effective in the formation of hemorrhoidal cones.
It is applied to the place where it is bleeding for several minutes. During this time, the sponge becomes saturated with blood and increases in size, while the vessels are compressed and the bleeding stops. The sponge has antiseptic, anti-inflammatory and healing effects.
Important information: On what day after conception does implantation bleeding occur and how many days does it last?
After providing emergency assistance and stopping the bleeding, you must contact a specialist who will help identify the cause of the pathology and eliminate it.
Intestinal polyps
Polyps are considered benign intestinal growths. They are mushroom-like formations on a stalk. Sometimes the patient does not even realize that he has a polyp.
In exceptional cases, polyps can develop into tumors. The surface of the polyp itself may begin to bleed. When the polyp reaches a large size, in most cases it begins to bleed, which leads to bleeding from the anus.
We present to your attention an additional article about the causes of pain in the anus in men.
Ischemic colitis and proctitis
We are talking about intestinal inflammation, which is caused by a lack of oxygen and nutrients entering the intestinal wall. Manifestations depend on the degree and rate of intestinal hypoperfusion. Typical symptoms include abdominal pain, which may be associated with nausea and vomiting. The urge to defecate and diarrhea occur relatively often, and blood is released from the anus (also present in the stool).
In severe forms, toxic megacolon and ileus (obstruction) develop with cessation of intestinal activity. Different parts of the large intestine begin to die. The disease is manifested by fever and the gradual development of peritonitis with sepsis. The result is shock and death.
For milder forms of the disease, conservative treatment is used. The patient is given intravenous fluids, usually avoids oral intake to minimize bowel irritation (with the possible provision of special intravenous nutrition), and is prescribed antibiotics. If it worsens, surgical removal of the affected part of the intestine may be necessary.
If intestinal necrosis is detected during colonoscopy, surgery is performed at any time and as soon as possible.
One of the main complications that can occur in both adults and children is short bowel syndrome, which occurs after these operations. Typical manifestations of proctitis are:
- mucous or purulent discharge from the anus;
- bleeding during stool.
Discharge from the anus in women is accompanied by painful sensations in the perineal area, which can radiate to the labia. Pain during bleeding from the anus in men often radiates to the scrotum area. These symptoms may include discomfort and the following signs:
- feeling of fullness in the rectum;
- frequent or constant urge to defecate;
- itching or pain in the rectum, especially during bowel movements.
Less common symptoms include cramping on the left side of the abdomen and diarrhea. These manifestations are either chronic (chronic proctitis) or occur repeatedly (acute proctitis).
Blood due to diverticulosis
A disease in which even blood clots can come out of the anus is diverticulosis. This disease is characterized by the development of multiple pouches in the colon caused by an unhealthy diet lacking fiber. They can cause bleeding or inflammation (diverticulitis).
A special type of diverticulum that can cause bleeding in the gastrointestinal tract is Meckel's diverticulum. It is located in the small intestine in approximately 2% of people (including children) as a congenital malformation of the gastrointestinal tract.
Once established, diverticula cannot be treated conservatively until they disappear completely. If diverticulosis is present and not causing problems, the condition does not require treatment. However, complications of the disease require solutions. If there is bleeding, the problem can be resolved endoscopically, but diverticulitis can also be treated with antibiotics.
In case of repeated complications, when diverticulosis bleeds, along with the lack of possibility of an endoscopic solution, intestinal perforation and worsening of the disease, the first-line method is abdominal surgery with removal of part of the colon with the diverticulum.
Colon cancer
The cause of cancer is not as common as other diseases in which blood leaks from the passage or is seen in the stool, but it should always be kept in mind. Cancer is usually preceded by the presence of a benign polyp from which bleeding occurs. Initially, this problem can be resolved with a relatively simple procedure during a colonoscopy.
Due to the fact that we are talking about the colon, the blood that may flow is bright red. If the presence of scarlet blood in the stool occurs when the patient is advanced in age, accompanied by weight loss and alternating diarrhea and constipation, we are talking about a possible oncological neoplasm.
Treatment depends on the stage at which the cancer was discovered. At the initial stage of the degeneration of a polyp into a malignant tumor, the formation is correctly removed using a colonoscope (polypectomy). There is no need for surgery, and even general anesthesia is not necessary. For some time before the procedure, it is necessary to avoid taking blood thinning medications (Aspirin, Varifarin).
At a later stage, treatment decisions should be made jointly with the oncologist. The best choice is surgical removal of part of the intestine (sometimes accompanied by a temporary or permanent colostomy), and local lymph nodes are often removed and examined for metastases. Treatment may be completed with chemotherapy.
If blood is found in the stool, it is important to pay attention to the presence of other symptoms. The warning should be the fact of weight loss, loss of appetite, alternating diarrhea and constipation, the presence of jaundice, fever and abdominal pain.
Intestinal diverticulosis
With this pathology, pouches and protrusions form on the intestinal walls. This could cause weakness in the intestinal wall. Diverticulosis can also develop when pressure in the abdominal cavity increases. Basically, these sacs - diverticula - do not cause discomfort.
But when the sac ruptures and the inflammatory process begins, it is characterized by the following condition:
- The patient's temperature rises;
- The muscles in the lower abdomen tense;
- Bleeding appears;
- Sometimes, depending on the part, the blood may be scarlet or dark red;
- This condition is quite serious and requires immediate surgical intervention.
Classification by blood color
Depending on the structure and color of the blood, we can talk about various diseases of the gastrointestinal tract. For example, the rich burgundy color of the liquid indicates the possibility of inflammatory processes in the duodenum. This is confirmed by symptoms such as nausea, vomiting and diarrhea. Dark red discharge indicates a hardening of the protrusion in the large intestine.
At the initial stage of the disease, symptoms are practically not felt. But as soon as the disease becomes active, pain is inevitable. Scarlet drops on toilet paper are harbingers of hemorrhoids. And if red spots are visible on your underwear, there is a high probability of malignant neoplasms.
Tarry stools indicate an exacerbation of stomach ulcers and gastritis. In this case, black blood flows from the anus.
Infection
An intestinal infection develops when various pathogens enter it.
There are the following types of infection, which are divided according to the location of the process:
- Colitis;
- Pancreatitis;
- Duodenitis;
- Gastritis.
Causes:
- Water containing microbes;
- Poor quality products;
- Poor personal hygiene;
- Communication with an infected person;
- Expired food products;
- Working on the ground.
Almost all intestinal infections are accompanied by the development of the following symptoms:
- Abdominal pain;
- Increased gas formation;
- The temperature rises;
- Nausea and vomiting appear;
- Diarrhea.
You cannot treat the infection on your own . Disordered stools, especially those mixed with blood, lead to dehydration.
Diagnostic methods
If drops of blood are detected in the stool, you should contact the clinic as soon as possible for urgent diagnosis. First of all, you should visit a proctologist. He will study the complaints, conduct an examination and palpation examination. If the blood is the result of hemorrhoids or cracks in the passage, then this can be detected with a standard palpation procedure.
But further examination of the condition of the intestines and other organs may be necessary; tests will be prescribed for this. Mandatory stool tests include tests for helminthic eggs and the presence of occult blood.
The doctor can make his final verdict and correct diagnosis after sigmoidoscopy. This examination helps to study the condition of the lower regions of the intestine using a device - an endoscope. The doctor inserts a thin tube into the anus, with a camera attached to the end. The doctor observes everything that happens inside on the monitor screen. The camera insertion limit is 30 centimeters long. But often this value is enough to determine the disease. In general, the procedure is not dangerous and has virtually no contraindications. The only exception when sigmoidoscopy cannot be performed is when the blood flows profusely and is difficult to stop, because in this condition the doctor will not be able to obtain reliable information, and even risks causing injury to the intestinal walls.
Diagnostics
You need to carefully prepare for an examination using an endoscope. So that the doctor can examine everything in detail, the intestines should be completely cleared of feces. Therefore, you will have to go on a diet for several days before the procedure, and in the morning before going to the laboratory, give an enema or take a laxative at night.
Digestive diseases
When the digestive system malfunctions, diseases begin to appear.
There are several most common diseases of the digestive tract:
- Gastritis;
- Dysbacteriosis;
- Stomach and duodenal ulcers;
- Colitis;
- Gastroduodenitis;
- Reflux – esophagitis;
- Cholecystitis;
- Pancreatitis;
- Constipation;
- Diarrhea.
Causes:
Poor quality food;- alcohol abuse;
- stress and depression;
- smoking;
- taking medications for a long period;
- heredity;
- Decreased immunity;
Symptoms:
- Pain of varying localization and intensity;
- Soreness can radiate to various organs and systems;
- The patient's appetite decreases;
- Heartburn and belching appear;
- Nausea and vomiting;
- Increased flatulence;
- Constipation or diarrhea.
Treatment of diseases of the digestive tract is based on taking medications to reduce inflammation and pain. Also, together with the medicine, the patient is prescribed a special diet.
Methods for treating bleeding from hemorrhoids
Treatment of hemorrhoidal bleeding is a whole complex of therapeutic methods. Therapy is aimed at eliminating the main symptom, inflammation, and normalizing stool.
The basis of treatment is proper nutrition. Eating vegetables and fruits with a high fiber content helps normalize intestinal function and eliminate constipation. Well-cooked meat, jellied meats, jellies improve the condition of the walls of blood vessels.
Diet alone cannot cure pathological changes in the vein; the use of medications is necessary. The types of medications are selected individually by the doctor based on the results of a physical examination and tests. The duration of the course depends on the clinical picture of the disease and the body’s response to therapy.
Despite the skepticism of doctors towards alternative medicine, folk remedies have proven their effectiveness in the treatment of hemorrhoidal bleeding. But folk recipes should be used as a supplement to therapy prescribed by a doctor.
Be sure to read:
How to quickly cure hemorrhoids: 2 effective methods + therapy at home
Oral anti-bleeding medications
Essentially, hemorrhoids are varicose veins of the anal canal, and bleeding is a complication of the disease.
As the basis of conservative therapy, angioprotective agents are prescribed in the form of tablets and capsules:
- Phlebodia 600;
- Vasocket;
- Venorutin;
- Troxerutin;
- Venolife Duo and others.
The drugs reduce the distensibility of the vessels of the cardiac system and venous stagnation. They increase the tone and frequency of capillary contractions, and improve microcirculation. Medicines have anti-inflammatory, vasoconstrictor effects.
Medicines are taken in courses. Most of them have contraindications and should be taken only as directed and under the supervision of a specialist.
Rectal suppositories and suppositories
Preparations for topical use, unlike tablets, act immediately on the affected area. This ensures higher efficiency and reduces the likelihood of side effects from the gastrointestinal tract.
Candles and suppositories are used for both internal and external hemorrhoids:
- Relief (alpha-adrenergic agonist) has a local vasoconstrictor effect. Reduces exudation, swelling, itching, irritation.
- Natalsid (coagulant) helps stop bleeding, eliminates inflammation, and accelerates the healing process.
- Parembal (angioprotector) has an enveloping anti-inflammatory effect.
- Anestezol (anesthetic and antiseptic in one) has a drying, astringent effect.
- Ginkor procto (angioprotector) reduces the fragility and permeability of blood vessels, improves microcirculation, and tones the veins.
Some medications are available in several dosage forms. Only a doctor can determine which form is optimal for a particular patient.
Ointments for hemorrhoids with blood
Ointments are prescribed for external hemorrhoids or if the patient has contraindications to suppositories:
- Trombless relieves pain, relieves swelling, and prevents the formation of blood clots.
- Proctosan accelerates healing and reduces inflammation.
- Hepatrombin N has a venosclerosing, antithrombotic effect.
- Bezornil is a complex drug with a hemostatic, countercurrent, astringent effect.
Ointments are usually applied twice a day after bowel movements.
Treatment of hemorrhoidal bleeding with folk remedies
Blood from hemorrhoids has been troubling humanity for many centuries. People have long found effective homemade remedies that they still use today.
- Sitz baths with herbs. Chamomile, calendula, and witch hazel are taken in equal proportions, poured with boiling water and infused. The strained solution is added to baths of warm water. 10-minute procedures are carried out daily for 10 days.
- Candles . Spring buttercup, peony petals are passed through a meat grinder and mixed with sea buckthorn oil. Form candles and put them in the refrigerator. Insert one every day for 2 weeks.
Be sure to read:
How to remove hemorrhoids: symptoms and treatment of external and internal nodes
If there is no opportunity or desire to prepare the remedies yourself, homeopathic medicines can be purchased at the pharmacy. Esculus ointment, Avenok plus suppositories, and Fleming ointment have proven themselves well.
Blood from the anus in men
Causes of bleeding from the anus in men:
- Haemorrhoids;
- Anal fissure;
- Intestinal polyp;
- Intestinal diverticulosis;
- Rectal cancer;
- Crohn's disease;
- Intestinal infection.
It is quite difficult to independently determine the cause of blood from the anus. To establish an accurate diagnosis and cause of the pathology, it is necessary to undergo an examination. Many men believe that blood is just the cause of hemorrhoids and put off visiting a proctologist. But this is a serious symptom that can eventually develop into cancer.
Gastric and duodenal ulcers and erosive gastritis
Causes peptic ulcers of the stomach and duodenum, as well as erosive gastritis for the following reasons:
- Helicobacter pilari bacillus;
- increased acidity;
- long-term use of non-steroidal, anti-inflammatory drugs;
- unbalanced diet;
- smoking;
- alcohol abuse.
An accurate diagnosis is established after fibrogastroduodenoscopy.
Symptoms:
- Pain in the epigastric region;
- Typically, pain is characterized immediately after eating or on an empty stomach;
- Flatulence;
- Bloating;
- Belching and heartburn.
Intestinal and other infections
An intestinal infection is characterized by the following symptoms:
- Loose stools mixed with mucus and blood;
- Nausea and vomiting;
- Temperature increase.
The cause of such symptoms may be salmonellosis, dysentery, or infestations.
Tumors of the digestive organs
The most common tumors of the digestive organs are:
- Stomach cancer;
- Bowel cancer.
Risk factors:
- Heredity;
- Smoking;
- Helicobacter pilari bacillus;
- Unbalanced diet;
- Consuming a small amount of plant fiber;
- Intake of refined foods;
- Polyps.
Varicose veins of the esophagus
Varicose veins of the esophagus are characterized by a violation of the outflow of blood from the veins of the esophagus. According to statistics, the age of this pathology occurs at 50 years. This occurs more often in men than in women.
Causes:
- Hypertension in the portal vein basin;
- Cirrhosis of the liver. Its symptoms in men are highlighted here.
- Hepatitis; We present to your attention an article about the first symptoms of hepatitis C here.
- Disease of the heart and blood vessels;
- Tuberculosis.
Symptoms:
- Belching;
- Heaviness in the chest;
- Heartburn;
- Nausea and vomiting.
Inflammatory bowel diseases
Nowadays, pathologies such as ulcerative colitis and Crohn's disease are quite common.
These are different diseases, but they have the same symptoms:
Pain and colic on the right and left sides of the abdomen;- Presence of feces in the blood;
- Bleeding from the anus;
- Dehydration;
- Loss of body weight;
- Damage to the eyes, liver, heart, blood vessels;
- Skin rashes;
- Thromboembolic complications.
Gastric bleeding: how to distinguish it from hemorrhoids?
Unfortunately, some patients do not react in any way to such a rather dangerous symptom as blood clots after bowel movements. This is due to the fact that pain is not always present with hemorrhoidal bleeding. Therefore, people think that nothing bad is happening in the body and do not seek help from a doctor. However, this is a very big mistake that can lead to serious consequences, the development of more severe stages of pathology and even death.
There is an explanation for such serious complications - quite often people confuse hemorrhoidal bleeding with bleeding of the gastrointestinal tract. To distinguish them, you need to pay attention to the color of blood clots. Thus, the shade of bloody discharge varies depending on which part of the gastrointestinal tract the problem occurs in.
Blood loss in the rectum or sigmoid colon has a bright color tint. In case of gastric or esophageal bleeding, the clots will appear darker in color.
It is important that if fermented food was present in the diet, the color of blood clots can be significantly distorted, which can mislead both the patient and the attending physician. In any case, it is impossible to do without specialized extensive diagnostics to clarify the specific diagnosis that provoked the blood loss.
Scarlet blood during bowel movements
Scarlet blood is usually found not in stool, but on toilet paper after a bowel movement. A bright scarlet hue indicates the development of the disease in the colon area, as well as possible damage to the tissues of the anus.
Along with this, a number of unpleasant signs appear, including pain and a feeling of increased pressure in the rectum. This situation may be caused by the following reasons:
- hemorrhoids - in this case, the bleeding is not profuse, mixed with feces and mucus clots, and may appear in the form of a small stream of blood. Usually occurs due to too hard stools or their large accumulation. If left untreated for a long time, pus may appear along with blood;
- diverticula of the intestinal region - heavy blood loss, which occurs with some frequency, often occurs in the period after childbirth and in elderly people
- fissures in the anal area - severe pain, copious amounts of blood clots;
- polyps in the rectum - bleeding can be painless, quite rare, along with this, mucus can be observed in the stool.
Blood during diarrhea
Liquefaction of stool along with blood during bowel movements in women and men is a very alarming symptom. In such cases, serious diseases such as salmonellosis, enteritis and internal hemorrhoids cannot be excluded.
When such diseases occur, the following signs may be observed:
- increased body temperature;
- vomiting and nausea;
- pulling pain that appears in the peritoneum;
- chills or, conversely, fever (which is extremely rare);
- profuse itching and burning sensation in the anus.
With severe darkening of the stool, the formation of various tumors, possibly even gastric ulceration, is possible. Loose stools with blood in women and men may indicate that the patient has:
- intestinal dysbiosis;
- food poisoning;
- helminthiasis and infection with other parasites;
- dysentery;
- ulcerative colitis;
- oncology in the rectal area.
If such a serious symptom as blood during diarrhea appears, you must consult a doctor as soon as possible, undergo a thorough examination and a series of laboratory tests.
Bleeding is a sign of anal fissures
Often hemorrhoids are accompanied by constipation and stagnation of feces, which subsequently becomes too dense and dehydrated. As a result, a person experiences severe pain during bowel movements, and with strong and prolonged straining, the rectal mucosa is injured, which can cause the formation of anal fissures on its surface.
The appearance of such a nuisance is often accompanied by symptoms such as severe pain during defecation, the appearance of blood clots and mucus from the anus, an open wound in the sphincter area, which can be seen upon examination, as well as a burning sensation and excessive pressure.
Important! If during the act of defecation a blood clot comes out of the anus, this indicates that the crack has risen higher, which requires urgent help. In this case, to stop blood loss, it is necessary to dry the wound, which is achieved by using local drugs.
Anal fissure is a risk of infection in the lower intestine. Therefore, proctologists usually prescribe disinfecting and healing suppositories and creams for anal fissures. The most popular of them:
- sea buckthorn suppositories;
- Heparin (ointment);
- Procto Glyvenol, etc.
To reduce pain, the use of suppositories containing an analgesic is required, the most popular of which are Relief. Thanks to the use of such local preparations, a protective film is formed on the rectal mucosa, which tightens and dries out cracks, destroys bacteria and accelerates the regeneration process.
VIDEO “WHAT CAUSES THE DISCHARGE OF BLOOD FROM THE ANUS?”
Bottom line
If there is minor bleeding from the anus, you must contact your local physician or proctologist and undergo an examination. Frequent bleeding can lead to anemia and the formation of a malignant tumor.
Mostly in men, bleeding is associated with hemorrhoids and anal fissure . If treatment is not started in time, the disease will become chronic and difficult to respond to treatment. When the bleeding is profuse and does not stop within 15 minutes, you need to call an ambulance and take the patient to the hospital.
Anal fissure is a common cause of bleeding from the anus.
An anal fissure is damage to the mucous tissue of the anus. The disorder is common in proctological practice and is detected very often among patients with hemorrhoids and other inflammatory diseases of the rectum.
The size of the crack usually does not exceed one centimeter, but despite this, the disease requires timely treatment. In especially severe cases, you even have to resort to the help of proctological surgeons. If an anal fissure is not treated, it can contribute to degenerative changes in tissue, the formation of polyps and increased inflammation.
Causes of anal fissures:
- chronic constipation;
- sedentary lifestyle;
- excess weight;
- anal injuries;
- chronic inflammation of the large intestine (hemorrhoids, proctitis, enterocolitis).
How does an anal fissure appear? It's hard not to notice her. The main symptom of the disease is a sharp pain in the anal fissure. When natural secretions come into contact with it, severe discomfort occurs. Urea further corrodes tissue, promoting the progression of the inflammatory process. After defecation, tonic contractions of the sphincter occur, which prevents the anal fissure from healing and completely disappearing. The spasm disrupts blood circulation in the tissues surrounding the anus, so regeneration slows down, and granulations begin to form near the fissure.
Painful sensations force the patient to deliberately avoid defecation, which leads to intoxication, chronic constipation and exacerbation of hemorrhoids. After 4-5 weeks, the fissure enters the chronic stage, its edges thicken, scar, and a characteristic “guard tubercle” appears, from which anal polyps can subsequently form.
Bloody discharge from a fissure in the anus is scant. Most often, patients find traces of blood on toilet paper or in stool. Chronic anal fissure is sometimes accompanied by anal itching. When sitting for a long time, patients feel discomfort, cannot do work for a long time and remain in the same body position.
What examination is prescribed for anal fissure?
For shallow and small cracks in the anus, proctologists perform a digital diagnostic method. But if the crack is very noticeable and bleeds, then this method is not used with preliminary anesthesia.
Instrumental diagnostics for sphincter spasm and severe pain due to a non-healing anal fissure are not carried out. In case of heavy bleeding, studies such as anoscopy, sigmoidoscopy may be prescribed, but only with the use of high-quality anesthesia.
How is an anal fissure treated?
In 70% of cases, anal fissure responds well to therapeutic treatment. Specialists eliminate sphincter spasms and constipation and ensure rapid tissue healing. Spicy foods, fatty foods, legumes, and alcohol are excluded from the patient’s diet. Warm anti-inflammatory baths with potassium permanganate, chamomile are prescribed locally, and botulinum toxin is used, which disrupts nerve conduction and relieves spasm of the rectal sphincter. Suppositories with hormones, anesthetics, and sea buckthorn oil are used. If therapeutic treatment is ineffective, the anal fissure is excised surgically.