ACE inhibitors (ACEIs) are the most prescribed group of drugs that lower blood pressure. Its representatives suppress the activity of one of the regulatory mechanisms that influence blood pressure levels - the renin-angiotensin-aldosterone system.
The first representative of angiotensin-converting enzyme inhibitors, captopril, was synthesized in 1975. The drug turned out to be so effective that it is still used today. Further study of the properties of captopril and its closest relatives made it possible to significantly expand the range of applications of the drug group.
Further study of the properties of captopril and the drug’s closest relatives made it possible to significantly expand the range of applications of the drug group.
Let's consider the mechanism of action, features of drug prescription, main side effects, absolute and relative contraindications.
pharmachologic effect
Regulation of blood pressure (BP) is a complex process that involves several biological mechanisms. One of them is the renin-angiotensin-aldosterone system. Angiotensin 2 and renin are two hormones that stimulate the contraction of blood vessels. Their lumen decreases, blood pressure increases. The mechanism of action of the drugs is simple: the substances block the conversion of the angiotensin precursor into its active form. A decrease in hormone concentration is accompanied by relaxation of the arterial wall and a decrease in blood pressure.
In addition to the main hypotensive effect, ACE inhibitors have additional beneficial properties that are used in the treatment of cardiovascular diseases and disorders. Conventionally, they can be divided into several groups.
| Effect type | The result of the influence of ACE inhibitors |
| Cardiovascular |
|
| Renal |
|
| Neurohumoral |
|
| Exchange |
|
| Anticipated Effects |
|
Video on the topic
This lecture presents the main pharmacological aspects of drugs acting on the renin-angiotensin-aldosterone system (ACE inhibitors, sartans and direct renin inhibitors):
ACE inhibitors are considered one of the most effective drugs that have a pronounced hypotensive effect. When used correctly and regularly, such medications will help lower blood pressure, restore kidney function, and normalize the condition of the heart and blood vessels. Like any other medications, ACE inhibitors cause side effects, so you need to take them carefully and not violate your doctor’s recommendations.
The information on the MyMedNews.ru website is for reference and general information, collected from publicly available sources and cannot serve as a basis for making a decision on the use of medications in the course of treatment.
MyMedNews.ru
And we also have
Calcium channel blockers, also known as calcium antagonists: classification, mechanism of action and list of drugs for hypertension
ACE inhibitors: classification
In the large pharmacological group of angiotensin converting enzyme inhibitors, there are several generations of drugs created at different times. Each new generation is safer and more effective, with fewer and fewer side effects. But in each category of drugs, regardless of the date of “birth,” there are leaders and outsiders, which must be taken into account when prescribing drugs to patients. All generations have their own niche of application, behave better or worse depending on the specific situation.
First generation
The very first drugs with a similar mechanism of action, known on the pharmacological market since the end of the last century. In modern medical practice, three types based on the sulfhydryl group are used:
- Captopril (Capoten, Blockordil, Angiopril) - used in emergency situations during hypertensive crises;
- Benazepril - has a milder effect, applicable for the correction of moderate hypertension, with heart failure;
- Zofenopril (Zocardis) is a first-generation drug with minimal negative consequences, prescribed at the onset of pathology.
The peculiarity of first-generation ACE drugs is their high efficiency with a large number of side effects. A precisely adjusted dosage is required. If used inappropriately, they provoke severe hypotension, up to a collaptoid state, and are excluded for self-medication.
First generation ACE inhibitors have:
- short-term action, quickly oxidize, excreted from the body;
- maximum bioavailability, which contributes to an immediate effect when taken.
They are removed mainly by the kidneys, so when prescribing, the functional safety of this organ is important.
Second generation
They are most actively used today throughout the post-Soviet space, they are distinguished by an optimal combination of safety and effectiveness while maintaining many undesirable side effects. They are represented by drugs with a carboxyl group as a base, such as:
- Enalapril (Vazolapril, Enalacor, Enam, Renipril, Renitek, Enap, Invoril, Corandil, Berlipril, Bagopril, Miopril);
- Perindopril (Perineva, Prestarium, Perinpress, Parnavel, Hypernik, Stopress, Arentopres);
- Lisinopril (Diroton, Irumed, Diropress, Liten, Sinopril, Dapril, Lysigamma, Prinivil);
- Ramipril (Dilaprel, Vazolong, Pyramil, Corpril, Ramepress, Hartil, Tritace, Amprilan).
A special feature is the use of ACE inhibitor drugs in complex therapy in older patients, since they are active in preventing thrombosis and the formation of cholesterol plaques. Used in all age categories to prevent the development of heart attack and stroke. When prescribed during the onset of arterial hypertension, they are considered the most effective and safe of the second generation ACE inhibitors. In the absence of renal pathology, they are considered the drugs of choice for the correction of cardiac diseases, since they are completely excreted in the urine. Distinctive features:
- high bioavailability, which is inferior to first-generation drugs, so peak activity in the body occurs half an hour after administration;
- The effect lasts longer (up to 8 hours).
Appointed for life.
Third generation
There are few long-term results with reliable clinical observations, so it is too early to talk about the best group of synthesized drugs. They use drugs based on the phosphinyl group for long-term use and treatment of chronic hypertension: Fosinopril, Monopril, Fosinap, Fosicard, Fozinotec, Ceronapril.
The peculiarity is that it is impossible to prescribe in emergency cases due to a long period of inertia before the onset of action, but the advantage is the choice based on the duration of the effect. It has been proven to have a mild effect on the patient’s body, with high efficiency and a minimal number of side effects. The downside is low bioavailability.
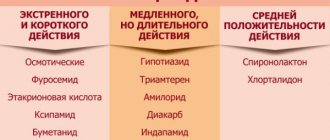
ACEIs can also be classified according to the frequency of taking drugs:
- short-term action - Captopril and its analogs: twice a day (sometimes increase the frequency to three doses);
- medium duration – Enalapril: taken no more than a couple of times a day;
- prolonged – Lisinopril: single dose.
Another approach to classification is clinical-pharmacological. Drugs of classes I and III are excreted in the urine, and drugs of the second class are excreted in urine or feces. The doctor takes this information into account when prescribing medications to people with liver or kidney diseases: functional organ failure can lead to the accumulation of active substances.
Clinical and pharmacological classification according to L. Opie
| Number, class name | Representatives |
| Class I – fat-soluble active dosage forms | Captopril |
| Class II – fat-soluble prodrugs | |
| ІІА - excreted mainly by the kidneys | Enalapril, quinapril, perindopril, cilazapril |
| IIB – excreted by the kidneys and liver | Ramipril, moexipril, fosinopril |
| ІІС - excreted mainly by the liver | Spirapril, trandolapril |
| Class III – water-soluble active dosage forms | Lisinopril |
inhibitors
INHIBITORS (from Latin mhibeo - I stop, restrain)
substances that inhibit chemical reactions. Inhibition is characteristic of catalytic and chain reactions that occur with the participation of active centers or active particles. The inhibitory effect is due to the fact that oxygen blocks the active centers of the catalyst or reacts with active particles to form low-active radicals that are unable to continue the chain. I. is introduced into the system in a concentration much lower than the concentration of the reacting substances (10−2–10−5 mol%). The kinetics of reactions involving iron are fundamentally different for catalytic and chain reactions. In catalytic reaction, the number of active centers is fixed and the enzyme, blocking some of them, is not consumed during the process. Therefore, with the introduction of I., the reaction rate decreases, and then the process takes a long time. time at a constant speed. In some cases, this speed may slowly increase due to the consumption of I. by sq.-l. adverse reaction. In a chain reaction, active particles are continuously generated, which leads to energy consumption and gradual self-acceleration of the reaction (in the case of a non-branched chain reaction, the original speed is usually restored).
Inhibition of chain reactions. Duration t of the braking action I. called. induction period; the number of chains f that one molecule breaks, sequentially entering into termination reactions called. stoichiometric coefficient inhibition. At the initial concentration of I. [I]0 and the rate of initiation of chains vi, the induction period is equal to: t = f [I]0/vi. For example, quinone inhibits the polymerization of vinyl monomers by entering into the trace. reactions:
In this case, f = 2 and t = 2[I]0/vi. In some systems, iodine is regenerated in chain termination reactions, as a result of which one iodine molecule and the radical formed from it repeatedly participate in termination reactions. For example, when copper ions are introduced into oxidizing isopropyl alcohol, the chains break as a result of a trace. alternating reactions:
In such systems, induction periods much exceeding 2[I]0/vi are observed. For each reaction there is a specific one. set I.: the reaction of hydrogen with chlorine is inhibited by NCl3 and O2, which react with chlorine atoms; polymerization of vinyl monomers - quinones, nitro compounds, I2, stable radicals (diphenylpicrylhydrazyl, nitroxyl radicals) that accept alkyl macroradicals; oxidation of org conn. (hydrocarbons, rubbers and polyolefins) phenols, aromatic. amines, aminophenols, reacting with peroxyl radicals RO2; cracking of hydrocarbons, olefins and nitrogen oxides reacting with alkyl radicals. To extinguish fire org connection. halohydrocarbons CF3Br, CF2ClBr, C2F4Br2 are used. Their inhibitory effect is caused by the fact that the branching agents during combustion are H atoms, with which I. react: RBr + The resulting HBr causes additional. chain break for reactions:
(M is any third particle). To extinguish fires, fire extinguishing powders are also used (for example, NaHCO3, phosphorus-ammonium salts), which have a combination. action: reduce the concentration of radicals due to intense chain termination on the surface and cause an increase. heat sink (see combustion). There are weak and strong I. of this reaction. A strong chemical is considered to be the one that, if introduced in a sufficiently high concentration, shortens the chain length to unity or reduces the reaction rate by v0/vi times, where v0 is the initial reaction rate. Weak I., even introduced in a relatively high concentration, reduces the reaction rate from vi to a certain value v > vi. This is due to the fact that radicals are formed from weak oxygen molecules that can continue the chain, due to which the ratio v0/v decreases with increasing [I]0, without reaching the value v0/vi. I., which has a strong inhibitory effect in a small concentration, is called. effective. The effectiveness of I. is characterized by the value of the derivative -dv/d[I]. For example, the oxidation of hydrocarbon RH in the presence of an initiator that creates the initiation rate vi is determined by the rate of chain continuation with the participation of the peroxyl radical:
so the initial rate of chain oxidation is v = kp. [RH] []. In presence I., for example, phenol, the chains are terminated by a product-type reaction. Under quasi-stationary conditions, the initiation and termination rates are equal: vi = fkt[I][RO2], therefore [] = vi/fkt [I] and v = kp[RH]vi/fkt [I]. The effectiveness of inhibition is characterized by the value of the fkt/kp ratio. Critical characteristics are characteristic for inhibition of branched chain reactions. phenomena, the essence of which is a sharp decrease in the reaction rate with very little. increasing the concentration of I. An example is inhibitor. autoxidation of hydrocarbons RH, in which bas. the source of radicals is the oxidation product ROOH. At a sufficiently high temperature or in the presence of a catalyst that intensively converts ROOH into radicals, the oxidation of RH can occur in a quasi-stationary regime, when the rate of ROOH formation is almost equal to the rate of its consumption. Because the rate of formation of ROOH depends on both the concentration of I. and the concentration of ROOH; there is some criticality. I. concentration, at which the system passes from a non-stationary to a quasi-stationary mode with a very slight (0.1–1%) change in I concentration. This is expressed in a sharp change in the reaction rate or induction period of I. Two I. introduced into the reacting system, can mutually enhance the inhibitory effect of each other (the so-called I. synergism) or weaken it (I. antagonism); an additive effect of two I. is often observed. If t1 and t2 are the duration of the inhibitory action of the first and second I., introduced separately, and t12 is the duration of their combined action, then in the case of synergy t12 > (t1 + t2), in the case of antagonism t12 < (t1 + t2). In the t-concentration diagram, in the case of synergism, a maximum is observed. Synergism I. can be due to either various. mechanisms of the inhibitory action of I. (for example, when inhibiting the oxidation of RH, one I. breaks the chains, and the other destroys ROOH), or chemical. interaction between two I. or the products of their transformation.
Inhibition of heterogeneous catalytic reactions is carried out by substances that are called. catalytic poisons. The inhibition of the reaction is due to a decrease in the activity of the catalyst due to the adsorption of oxygen on its surface.
Inhibition of enzymatic reactions may. reversible and irreversible. In both cases, I. is capable of forming a complex with the enzyme, but cannot. subjected to catalytic transformation and prevents the formation of the enzyme-substrate complex. For example, butanol inhibits carboxypeptidase-catalyzed ester hydrolysis. There are traces. cases of reversible inhibition. Direct competitive inhibition, in which molecules I. I and substrate S compete for attachment to the active center of enzyme E. The process is described by the relationships (P is the transformation product):
With this braking mechanism, if [E] << [S]0 and E << [I]0, the initial speed turns. substrate S is equal to:
Non-competitive inhibition, in which I. joins an active enzyme or a complex of an enzyme with a substrate to form a catalytically inactive form:
In this case, the initial reaction rate is:
Non-competitive inhibition, in which I. forms a catalytically inactive complex with the substrate:
The initial reaction rate is:
There have been cases of enzyme inhibition by a substrate, when a second molecule of the substrate forms an inactive complex with the enzyme (substrate inhibition). Irreversibly reacting enzymes react with the enzyme, deactivating it; in contrast to reversible inhibition, enzyme activity decreases over time.
Application. Inhibition is widely used to control the rate of radical polymerization, in particular when producing large volume products. I. oxidation is used to stabilize polyolefins and rubbers during their processing and under operating conditions (see destruction of polymers), to stabilize lubricants and hydrocarbon fuels, and to preserve food. fats and drugs drugs; in monomer production technology they are used to prevent oxidation. polymerization. In research works, I. are used to study the mechanism of chain reactions, in particular to determine the rate of initiation.
Lit.: Ashmore P., Catalysis and inhibition of chemical reactions, trans. from English, M., 1966; Webb L., Enzyme and Metabolism Inhibitors, trans. from English, M., 1966; Kuliev A.M., Chemistry and technology of additives for oils and fuels, M., 1972; Denisov E.T., Kovalev G.I., Oxidation and stabilization of jet fuels, M., 1983.
E. T. Denisov
Source: Chemical Encyclopedia on Gufo.me
Meanings in other dictionaries
- inhibitors - Inhibitors are substances that block certain parts of the metabolism of a living organism, thereby suppressing its development. Explanatory dictionary of soil science
- inhibitors - inhibitors plural. 1. Substances that slow down the progress of chemical reactions (up to their complete cessation). 2. Substances that inhibit enzyme activity. 3. Antihypertensive drugs that help equalize blood pressure without allowing it to rise sharply. Explanatory Dictionary by Efremova
- inhibitors - Chem. substances that reduce the rate of biochemical reactions or suppressing them by acting on the corresponding enzymes. I. are used as medicines (for example, sulfonamides), pesticides, and also in studying the metabolism of living organisms (inhibitory analysis). Microbiology. Glossary of terms
- inhibitors - (INHIBITORY SUBSTANCES). Collective name for chemical substances and compounds... Culinary Dictionary
- Inhibitors - I Inhibitors (from Latin inhibeo - stop, restrain) in biology, natural and synthetic substances that inhibit the activity of enzymes (both in a living organism and in cell-free systems); differ in the nature of action, specificity, etc. Great Soviet Encyclopedia
- inhibitors - (from Latin inhibeo - restrain, stop), decomposed substances. chemical nature, suppressing catalytic. activity of the department enzymes or enzyme systems. Along with repressors of enzyme synthesis... Biological encyclopedic dictionary
- INHIBITORS - INHIBITORS (from the Latin inhibeo - I hold) - substances that reduce the rate of chemical, including enzymatic, reactions or suppress them. Large encyclopedic dictionary
- Blog
- Jerzy Lec
- Contacts
- Terms of use
© 2005—2020 Gufo.me
List of the best drugs and their names
Of the entire extensive group of drugs, 5 drugs are most often used: captopril, ramipril, fosinopril, enalapril, lisinopril. All of them are well tolerated and have features that make them more popular.
Active substance, trade names, characteristic features:
- Captopril (Blocordil, Capoten). The only drug used to relieve hypertensive crisis. Suitable for most patients.
- Ramipril (Amprilan, Dilaprel, Pyramil, Hartil). Pronounced hypotensive effect, convenient dosage regimen.
- Fosinopril (Monopril, Fosicard, Fosinap, Fozinotec). Representative of the latest generation. Has the most pronounced hypotensive effect. Suitable for patients with severe renal failure.
- Enalapril (Berlipril, Renipril, Renitek, Ednit, Enap). Inexpensive, effective, safe.
- Lisinopril (Dapril, Diropress, Diroton, Irumed, Lizacard, Lysigamma, Lisinoton, Lizoril). Does not accumulate in adipose tissue: the optimal choice for excess weight and metabolic syndrome.
ACE inhibitors - indications for use
The use of these medications is necessary, first of all, for people who have:
- chronic heart failure;
- dysfunction of the left ventricle;
- diabetic nephropathy;
- survivors of a heart attack.
Failure to prescribe this category of patients is associated with a poor prognosis. Such readings are called absolute.
The appointment of an ACE inhibitor is justified, but not necessary, when:
- stable coronary heart disease (CHD), especially if there are absolute indications;
- myocardial infarction;
- systemic atherosclerosis;
- renal dysfunction of non-diabetic origin;
- severe atherosclerotic damage to the heart vessels.
Myocardial infarction
The administration of ACE inhibitors to patients who have suffered a heart attack can significantly reduce the mortality rate (1). It has been proven that drugs are especially important if the patient has dysfunction of the left ventricle, obvious/hidden heart failure.
Most people start taking AFP blockers between days 3-10. This allows you to prevent a sharp drop in blood pressure and the development of complications. Earlier appointment is justified in patients with large-focal infarction of the anterior wall, recurrent heart attack.
The minimum duration of treatment is 6 months.
Arterial hypertension
ACE inhibitors are one of 5 groups of first-line drugs to combat hypertension. This means that they are suitable for the vast majority of patients and are recommended for use for this diagnosis in the first place. Medicines are prescribed to patients who have absolute indications.
Usually the drugs are taken together with antihypertensive drugs of other groups. The most effective combinations are ACE inhibitors + thiazide/thiazide-like diuretics/calcium antagonists. Isolated treatment is rarely used due to low effectiveness: only 50% of patients succeed in achieving a stable reduction in blood pressure. When hypertension and hypercholesterolemia are combined, patients are prescribed complex medications that, in addition to antihypertensive components, contain statins.
List of the best combination drugs
| Active substance | Tradename |
| Amlodipine + Atorvastatin + Perindopril | Lipertans |
| Amlodipine + Lisinopril + Rosuvastatin | Equamer |
| Amlodipine + Lisinopril |
|
| Amlodipine + Ramipril |
|
| Hydrochlorothiazide + Lisinopril |
|
| Hydrochlorothiazide + Enalapril |
|
Blood pressure does not decrease immediately when taking medications. Maximum results are achieved in 2-4 weeks. There are 2 options for the patient’s body’s reaction to taking pills, depending on the activity of renin.
| Renin activity level | Blood pressure reaction |
| High | 3 phases:
|
| Normal/low | Gradual decline |
Diabetes
Patients with diabetes are at risk of developing diabetic nephropathy and chronic renal failure. The use of ACE inhibitors can reduce it. At high creatinine levels (more than 300 µmol/l), they are recommended to be combined with loop diuretics and calcium antagonists. This helps prevent the development of unwanted reactions.
Medicines in this group are prescribed even to people with normal blood pressure if they have signs of kidney damage - albumin excretion in the urine (albuminuria).
At the initial stage of prescribing antihypertensive drugs, it is necessary to more carefully monitor blood sugar concentrations. This requirement is explained by the effect of ACE inhibitors on the mechanism of glucose uptake. The drug increases tissue sensitivity to insulin, which promotes the absorption of sugar. This can cause hypoglycemia (low glucose levels).
Raas blocker drugs
The renin-angiotensin-aldosterone system
(
RAAS
) regulates blood pressure, as well as sodium and water homeostasis.
Renin
synthesized by specialized smooth muscle cells in the wall of the afferent arteriole of the renal glomerulus (juxtaglomerular apparatus). Renin release may be due to a fall in renal perfusion pressure and sympathetic activation of β-adrenergic receptors in juxtaglomerular cells.
As soon as renin
enters the blood, it breaks down angiotensinogen synthesized in the liver to the decapeptide angiotensin I. ACE, in turn, converts angiotensin II into biologically active angiotensin II.
APF
, circulating in plasma, is localized on the surface of endothelial cells. It is a nonspecific peptidase capable of cleaving C-terminal dipeptides from a variety of peptides (dipeptidyl carboxypeptidase). Thus, ACE helps inactivate kinins such as bradykinin.
Angiotensin II
can activate two different receptors (AT1 and AT2) coupled to G proteins. The most significant effect that angiotensin II has on the cardiovascular system is mediated by AT1 receptors. Angiotensin II increases blood pressure in various ways: 1) vasoconstriction of both the arterial and venous beds; 2) stimulation of aldosterone secretion, leading to an increase in renal reabsorption of NaCl and water, and consequently to an increase in blood volume; 3) central increase in the tone of the sympathetic nervous system, and in the periphery - increased release and action of norepinephrine. Long-term increases in angiotensin II levels can lead to hypertrophy of the muscle cells of the heart and arteries and an increase in the amount of connective tissue (fibrosis).
a) ACE inhibitors
, such as captopril and enalapril, occupy the active site of this enzyme, competitively inhibiting the breakdown of angiotensin I. These drugs are used for hypertension and chronic heart failure. The reduction in elevated blood pressure is mainly due to a decrease in the formation of angiotensin II. A weakening of the breakdown of kinins that have a vasodilatory effect may also contribute.
For congestive heart failure
after the use of an ACE inhibitor, the cardiac output increases, because due to a decrease in peripheral resistance, the afterload of the ventricles decreases. Venous congestion (preload) is reduced, aldosterone secretion and the tone of venous capacitance vessels are reduced.
Side effects
. If activation of the RAAS is due to loss of electrolytes and water (as a result of treatment with diuretics, heart failure or renal artery stenosis), the use of ACE inhibitors may initially cause an excessive drop in blood pressure. Quite often, a side effect such as a dry cough (10%) is observed, the cause of which may be a decrease in the inactivation of kinins in the bronchial mucosa.
Combination of ACE inhibitors
with potassium-sparing diuretics can lead to hyperkalemia. In most cases, ACE inhibitors are well tolerated and provide a good therapeutic effect.
Towards new analogues of these drugs
include lisinopril, ramipril, quinapril, fosinopril and benazepril.
b) Antagonists of AT1 receptors of angiotensin II
("
sartans
"). Blockade of AT1 receptors by antagonists suppresses the activity of angiotensin II. The first drug in the “sartan” group was losartan, and analogues were soon developed. These include candesartan, eprosartan, olmensartan, telmesartan and valsartan. The main (hypotensive) effects and side effects are the same as for ACE inhibitors. However, “sartans” do not cause a dry cough, because they do not inhibit the breakdown of kinins.
c) Renin inhibitor
. Since 2007, a direct renin inhibitor (aliskiren) has been available on the market and can be used to treat hypertension. This drug is poorly absorbed after oral administration (bioavailability 3%) and is excreted very slowly (half-life 40 hours). Its spectrum of action is similar to AT1 receptor antagonists.
Main advantages
The main advantages of ACE inhibitors (4):
- good tolerance;
- minimum of adverse reactions, contraindications;
- suitable for patients with diabetes, kidney disease, and the elderly;
- do not affect heart rate;
- a large number of useful auxiliary effects;
- with long-term use, they reduce the incidence of cardiovascular complications and increase life expectancy;
- do not interfere with erection;
- do not impair exercise tolerance;
- help improve cognitive functions in elderly patients;
- relatively low cost.
Possible side effects
The drugs are well tolerated by most people, which partly explains their widespread use in medical practice. The most sensitive to side effects are representatives of the Negroid, Mongoloid race.
The most common undesirable consequence of taking ACE inhibitors is a dry, paroxysmal cough. It affects 5-20% of patients (2). An unpleasant symptom usually occurs within a week to six months, more often in women, patients with renal failure and does not depend on the dose. The appearance of cough is explained by the accumulation of bradykinin, prostaglandins or substance P in the tissues of the upper respiratory tract.
Other possible negative reactions common to all ACE inhibitors:
- decreased blood pressure (hypotension);
- decreased plasma potassium concentration (hypokalemia);
- kidney dysfunction;
- perversion of taste.
Captopril tablets contain a sulfhydryl group due to an additional list of side effects (3):
- skin rash;
- the appearance of protein in the urine (proteinuria);
- decreased neutrophil count (neutropenia).
The most dangerous negative effect is Quincke's edema. It develops in 0.1-0.2% of patients. The mucous membrane of the nose, mouth, pharynx, and larynx swells, and the person begins to choke. Such a negative reaction, like cough, is associated with the accumulation of bradykinin.
How do angiotensin converting enzyme inhibitors work?
The mechanism of action of ACE inhibitors can be briefly explained as follows. When an active substance from this group enters the body, its full list will be given below, it inhibits the production of exopeptidase.
This enzyme helps convert the inactive hormone angiotensin-1 into its active form, angiotensin 2, which narrows blood arteries. Thus, ACE inhibitors help normalize blood pressure.
On a note. For hypertensive patients with heart failure accompanied by moderate edema, in addition to ACE inhibitors, the doctor may prescribe carbonic anhydrase inhibitors - drugs that cope better with edema than thiazide diuretics. Their trade names are Acetazolamide, Diamox, Diacarb (active ingredient acetazolamide).
In addition, ACE inhibitors also reduce blood pressure by slowing down the breakdown and stimulating the synthesis of a special peptide - bradycardin, whose function is to dilate blood vessels. Moreover, when it breaks down, two substances are formed - nitric oxide and prostacyclin.
It is because of this that ACE inhibitors are the first choice drugs for lowering blood pressure in patients with type 2 diabetes mellitus, including those with “diabetic foot”.
ACE inhibitors can be taken by heart attack patients, hypertensive patients with CHF and left ventricular dysfunction
Prils also reduce the concentration of protein in the urine and help lower glomerular pressure. Therefore, angiotensin-converting enzyme drugs are indicated for the treatment of hypertensive patients with diabetic nephropathy or other chronic kidney pathologies.
Contraindications
There are two groups of warnings for use:
- absolute – conditions incompatible with the use of drugs;
- relative - the use of tablets is undesirable, but possible if the potential benefit outweighs the possible harm.
Complete list of contraindications for taking medications
| Absolute | Relative |
| Hypersensitivity to any component of the drug | Moderate arterial hypotension (systolic blood pressure 90-105 mm Hg) |
| Negative experience of receiving other representatives | Severe chronic renal failure (creatinine more than 300 µmol/l) |
| Pregnancy | Age less than 18 years |
| Feeding the baby | Gouty kidney |
| Bilateral narrowing of the renal arteries or unilateral if there is only one kidney | Women of childbearing age who are not using effective contraception |
| Severe low blood pressure (hypotension) | Chronic cor pulmonale, accompanied by edema, abdominal dropsy (ascites) |
| Severe form of narrowing of the aorta | Obliterating atherosclerosis of the legs |
| Plasma potassium content more than 5.5 mmol/l | Hemoglobin less than 79 g/l |
| Porphyria | |
| Neutropenia (less than 1000 cells/mm3) |
It is not advisable to take ACE inhibitors for people receiving immunosuppressants, drugs that suppress cell division. Taking these drugs together is dangerous due to a pronounced decrease in the number of leukocytes. Examples of undesirable combinations are allopurinol, phenothiazine, rifampicin.
Side effects
Despite being well tolerated, in some cases ACE inhibitors can cause side effects, such as:
- a sharp decrease in pressure;
- cough syndrome;
- spasms in the bronchi;
- hyperkalemia;
- kidney dysfunction;
- increased swelling;
- change in taste sensations;
- stomach pain;
- disorders of digestive processes;
- vomiting and nausea;
- diarrhea;
- liver pathologies;
- disturbances in the outflow of bile;
- itching and rashes on the skin;
- anemia;
- convulsions;
- decreased libido;
- general weakness;
- sleep disorders, etc.
Most often, side effects of ACE inhibitors occur due to improper use or overdose of medications.
Before starting treatment, the patient must make sure that there are no contraindications to the use of such medications. Patients often seek ACE inhibitors that do not cause coughing. According to statistics, in Europeans, when taking ACE inhibitors, side effects in the form of a dry cough occur in only 10% of patients. It is not recommended to take medications for diseases and symptoms such as:
- hypotension;
- aortic stenosis;
- renal artery stenosis;
- severe form of renal failure;
- hypersensitivity (intolerance) to the components of the drug;
- leukopenia;
- porphyria;
- hyperkalemia.
ACE inhibitors should not be used by young children, nursing mothers, or pregnant women. Expectant mothers should understand that drugs in this group can reduce the amount of amniotic fluid and also negatively affect the fetus, causing growth retardation and the development of congenital anomalies.
Literature
- I. Kuznetsov, N.B. Sturov. The use of ACE inhibitors and angiotensin II receptor blockers (sartans) in general medical practice, 2010
- A. G. Gilman. Clinical pharmacology according to Goodman and Gilman, 2006
- Orlov V.A., Gilyarevsky S.R., Urusbieva D.M., Daurbekova L.B. The influence of side effects of angiotensin-converting enzyme inhibitors on the treatment of cardiovascular diseases, 2005
- Yu.A. Karpov. Angiotensin-converting enzyme inhibitors and treatment of arterial hypertension, 2002
Irina Kostyleva
Higher medical education. Kirov State Medical Academy (KSMA). Local therapist. More about the author
All articles by the author
Mechanism of action
ACE inhibitors (this abbreviation stands for angiotensin-converting enzyme) are a group of medications that can block the formation of angiotensin, a hormone that accumulates in the blood plasma.
The mechanism of action of ACE inhibitors is that angiotensin constricts blood vessels, disrupts systemic blood flow and increases blood pressure. In addition, angiotensin stimulates the production of another hormone - aldesterone, which provokes the development of vascular spasms, fluid and sodium retention in the body, rapid heartbeat and some other symptoms that accompany arterial hypertension.
The mechanism of angiotensin formation is quite complex and is not always understandable to a person who has a superficial understanding of biology and chemistry. This substance arises as a result of many chemical reactions occurring in the human body.
Captopril tablets
Under the influence of adrenaline, the kidneys begin to produce the enzyme renin, which enters the systemic circulation and is converted there into angiotensinogen, which is also called angiotensin I. At the next stage, angiotensin I is converted into angiotensin II (angiotensin itself), this process is facilitated by a special angiotensin-converting enzyme, which inhibitor drugs act.
The first ACE inhibitors appeared more than 40 years ago. It was then that scientists managed to synthesize Captopril, which became one of the main drugs prescribed for high blood pressure. Captopril was replaced by Enalapril, Lisinopril and other new generation drugs.
Anaprilin is an adrenergic blocker of beta receptors of the first and second groups. The drug is prescribed for diseases that are caused by instability of vascular tone.
High blood pressure tablets Coronal are a reliable medicine widely used in cardiology. The drug reduces the manifestations of hypertension, coronary artery disease, and angina pectoris.