Types of cholesterol in the blood and why you need to know it
Correct judgments about cholesterol provide knowledge about it. Not all cholesterol causes harm, but only certain fractions of it. And the harm occurs not because these fractions are present in the body, but because the level is too high.
Total cholesterol is divided into:
- High density lipoproteins (HDL). This is “good” cholesterol. It is involved in the creation of new cells and promotes better absorption of vitamins. Also plays an important role in the formation of hormones and bile production. Thanks to this fraction, the elasticity of blood vessels increases, and the amount of excess cholesterol deposits decreases.
- Low density lipoproteins (LDL). This is “bad” cholesterol. Due to its excessive amount, the risk of developing atherosclerosis increases.
- Very low density lipoproteins (VLDL). This is the most atherogenic fraction. If this indicator is too high, then there are pathologies in the body.
- Intermediate density lipoproteins (IDL). They are a product of the conversion of VLDL to LDL. Act as triggers in the occurrence of heart and vascular diseases.
- Only the first faction from this list is good. The rest are “bad”. These indicators must be carefully monitored, not allowing them to go beyond the norm. The total cholesterol level is determined by the total value of all items from the list.
The functional state of the body depends on the study of all cholesterol fractions separately and on their total value .
Ways to check cholesterol
To find out the cholesterol level in your blood, you need to go to the clinic. This analysis is carried out in several ways. The choice depends on the purpose of the study.
Express test
You can purchase a special device for a quick blood test at home. This is a glucometer, usually used by diabetics to determine their glucose levels. But some devices can also measure cholesterol and triglycerides. To do this, a drop of blood is taken from a finger. It is applied to a special test strip and inserted into the analyzer. The result is ready in a few minutes.
This test does not determine cholesterol as accurately as in the laboratory. The cause of the error may be increased temperature or humidity, food eaten shortly before the test, or stress . But express diagnostics can be used to independently monitor your health status. If the results are concerning, you can go and get a full test.
General
The level of total cholesterol is usually determined by a biochemical blood test. It is measured in mmol/l. If the result form says mg/dL, you need to multiply this figure by 38.5. Designated TC or Chol.
Results of 2.9-5.2 mmol/l are considered normal. This means that the person is not at risk of cardiovascular disease. If the result is within 5.2-6.2 mmol/l, it is recommended to conduct an extended lipid profile, determining the amount of lipoproteins and triglycerides.
But this indicator depends on the age and gender of the person. For example, for men over 35 years of age, normal values will be up to 6.9 mmol/l, and after 45 years – 7.1 mmol/l. In women, its amount also increases with age: after 35 years, 6.2 mmol/l is the norm, and after 55 – 7.7 mmol/l.
Detection of lipoproteins
It is much more important than the level of total cholesterol to find out the content of different types of lipoproteins in the blood.
- HDL is sometimes designated by the letters HDL. They help prevent the development of atherosclerosis. Normally, their amount should be from 1 to 2 mmol/l. For men, the rate is lower - from 0.7 to 1.7, and for women - from 0.8 to 2.3. It is believed that the higher the amount of HDL, the lower the risk of developing cholesterol plaques.
- LDL or LDL is the most important indicator; it should be less than 4 mmol/l. When the amount increases, the development of atherosclerosis begins. But these indicators greatly depend on the age and gender of the person. After 30 years, results of 4.4-4.9 are considered normal, after 40 – 4.9-5.3, and after 50 – 5.3-5.7 mmol/l.
- Often the level of very low density lipoproteins – VLDL or VLDL – is also determined. They transport cholesterol molecules and serve to form LDL. Normally, their amount should be no more than 1 mmol/l. If more, cholesterol plaques will be deposited on the walls of blood vessels.
Triglycerides
This indicator is designated in the test results as TG or TRIG. Measured in mol/l. The amount of triglycerides in the blood should not exceed 1.77 mmol/l. If the indicator is 1.7-2.2 mmol/l, you need to follow a diet, 2.3-5.6 - treatment is required, since there is a high risk of developing heart and vascular diseases. If the amount of triglycerides is more than 5.6 mmol/l, not only the blood vessels are affected, but also the pancreas.
Lipidogram
If the results of the general analysis turn out to be threatening, the doctor gives a referral for a lipid profile. It includes the following indicators:
- THC – total cholesterol;
- LDL cholesterol – low density lipoproteins;
- HDL cholesterol – high density lipoproteins;
- TG – triglycerides;
- KA or IA – atherogenicity index.
The last indicator is even more important than the others. It allows you to estimate the ratio of HDL to other lipoproteins. The risk of developing cardiovascular diseases depends on this. AI is calculated as follows: the amount of HDL is subtracted from the total cholesterol and the resulting result is divided by HDL. An increase in this indicator to 4 is possible only in healthy men and women from 30 to 40 years old. If there is a risk of developing coronary heart disease, it should not be more than 3. It is dangerous when the AI is more than 5. This condition can cause vascular pathologies, kidney failure, and stroke.
Who should take a cholesterol test?
Previously, it was believed that all people needed to undergo a cholesterol test once every five years. It was then recommended that this analysis be carried out every three years.
Nowadays, the pace of life has accelerated. This led to poor nutrition. Obesity and other pathologies developed. Therefore, now absolutely everyone needs to undergo a cholesterol test once a year. Healthy people take this test for prevention.
It is also recommended to take the test:
- Pregnant women (often due to nutritional disorders, they have high levels, and the doctor adjusts the diet);
- People over forty years old with a high risk of developing coronary heart disease (they are shown a detailed analysis with indicators of all fractions);
- Patients with liver, kidney and pancreas diseases;
- People who are obese;
- During statin therapy.
Quality of life is determined by good health. Therefore, it is necessary to take time for yourself.
You need to examine your own body in time.
Norms
To decipher the indicators, you need to know how cholesterol in the blood is indicated? The designation of cholesterol in a blood test in adults and children depends on age. The amount of lipid in older people is higher as metabolism slows down. A breakdown of the blood test for cholesterol in adults is presented in the table. Patients should understand that the norm is different for each gender and age. Particular importance is attached to the cholesterol levels of pregnant women, because pregnancy is a period when the health of the child depends on the health of the mother.
Important! Excessively high levels of cholesterol in pregnant women are the cause of difficult labor. Bad cholesterol affects blood pressure, heart function, hormonal levels, etc.
Acceptable norms of total Chol (сholesterol) in the blood:
- newborn children – no more than 3.5 mmol/l,
- up to 1 year – 1.81 – 4.53 mmol/l,
- up to 12 years – 3.1 -5.18 mmol/l,
- 13-17 years – 3.11-5.44 mmol/l,
- in women and men – 3.6 – 5.2 mmol/l.
If we talk about LDL, then the indicators are different:
- for women – up to 3.5 mmol/l,
- for men – 2.25 – 4.82 mmol/l.
The attending physician must decipher the cholesterol in the analysis. You cannot independently establish a diagnosis, prescribe, cancel or increase the permissible dose of drugs. Changes in the dosage of medications that affect cholesterol levels may make the situation worse.
Advice! Any use of traditional medicine in the process of reducing LDL in the blood must be agreed with the attending physician.
Preparing for analysis
In order to find out the cholesterol level, the doctor sends the patient for a lipid profile. This is the most detailed analysis, allowing us to identify the indicators of all fractions and their ratio.
Before performing the test, the patient is given general recommendations:
- On the day of the test you cannot eat anything, you can only drink water. The test is performed on an empty stomach, so it is done in the morning.
- The day before you should not eat anything fatty, spicy or fried.
- Dinner on the eve of the study should be no later than 18:00.
- You should not drink alcohol before the test.
- If the patient takes certain medications, the doctor may stop them before the test.
- Smokers will have to give up cigarettes on the eve of the test.
- To prevent HDL levels from increasing, physical activity must be avoided.
Why is analysis necessary?
Many people use the word “cholesterol” to mean a substance harmful to the body. In fact, cholesterol is present in cells and is involved in important processes. In medicine, standards for its content in the blood have been determined.
It is important to monitor the indicators and not allow them to decrease or increase. Doctors recommend checking cholesterol once every five years, and after 40 years - once every three years.
Analysis is prescribed in a number of cases:
- during a preventive examination;
- during a clinical examination;
- for diagnosing liver pathologies;
- for diabetes mellitus;
- to control cholesterol dynamics during drug treatment;
- for diagnosing thyroid diseases;
- to diagnose lipid barrier disorders;
- for the diagnosis of atherosclerosis;
- when assessing the risks of strokes and heart attacks.
Note! Cholesterol is not indicated in a general blood test. To determine it, biochemical parameters are examined.
The study determines total cholesterol, as well as LDL, HDL and their ratio to each other. A lipidogram is needed to provide a complete picture of the patient’s health status.
Low-density lipoproteins (LDL), also known as bad cholesterol, are dangerous. They are practically insoluble and form plaques on blood vessels. Elevated levels increase the risk of heart attack, atherosclerosis and stroke.
High-density lipoprotein (HDL), in other words, good cholesterol, plays an important role in the functioning of the body. They get rid of bad cholesterol, promote the absorption of fat-soluble vitamins, prevent the formation of plaques, and participate in the production of hormones.
Total cholesterol is the sum of the two previous indicators. A low level may indicate lipid metabolism disorders, psychophysical disorders, an increased level may indicate the risks of atherosclerosis and diabetes.
A lipid profile can provide the most accurate information about your health status. It allows you to identify the disease and identify possible risks.
The lipid profile includes cholesterol (total, bad, good), atherogenicity coefficient and triglycerides.
Atherogenic index (AI) is the proportion of total cholesterol with HDL and LDL.
The indicator assesses the state of fat metabolism and shows the possible risks of cardiovascular pathologies, atherosclerosis, and plays a role in determining liver and thyroid diseases. With the help of AI, the dynamics of changes in cholesterol during drug treatment is monitored.
Triglycerides, otherwise neutral fats, are an important source of energy that comes with food and is synthesized in tissues. These compounds can provide additional information in the diagnosis of heart attacks, atherosclerosis, vascular thrombosis, coronary heart disease and a number of other diseases.
Blood testing for cholesterol
A century ago, zemstvo doctors judged a patient’s condition by the color of urine, or by the color of smears and sputum. Now medical technology has developed, and all tests are carried out in laboratories. Their results are so accurate that the error is less than a percent.
Laboratory doctors and specialists with higher medical or biological education perform their work with high efficiency and accuracy.
But the interpretation of the tests, their connection with pathological changes, continue to be studied to this day.
For analysis, blood is taken from a vein, as this allows for more accurate results. Blood is drawn using a disposable sterile syringe. Next, the blood is sent to the laboratory, where it is examined using a special analyzer. Test results can be obtained within a day.
To get quick results, you can use a rapid test. Also, portable express analyzers are good for those patients who need to constantly monitor their cholesterol levels by performing tests very often.
How to take a cholesterol test correctly
To determine the amount of cholesterol, venous blood is examined. You need to donate 5 ml from a vein. The procedure takes a few seconds, and the result is ready the next day or a couple of days later. At this time, the blood is examined using a special apparatus. The test is taken on an empty stomach , usually in the morning from 8 to 10 o'clock. But before it, preparation is necessary . There are certain rules that must be followed for the result to be reliable.
It is not recommended to donate blood after surgery, a heart attack, an exacerbation of a chronic pathology, or an acute illness. It is recommended to wait at least 6 weeks for your health condition to stabilize.
Diet before donating blood
The patient should know what not to eat or drink before donating blood for cholesterol. Since blood is tested on an empty stomach, you need to fast for 12-14 hours. In the evening at 7-8 o'clock, have a light dinner and eat nothing else. You can drink water, but all other drinks and foods can affect test results.
It is recommended to follow a diet a few days before donating blood. It is necessary to exclude fatty foods and fried foods from the diet. Limit the consumption of sweets, confectionery, spicy seasonings - that is, those foods that can affect lipid metabolism and liver function.
Preparing for analysis
In order for the results to be accurate, you need to know how to properly prepare for donating blood for cholesterol. It is advisable to do this in advance. If medications were prescribed to reduce its level, you need to stop taking them 2 weeks before the test. The doctor should also be warned about other medications you are taking, as many of them may affect the results. You should try to avoid, if possible, the use of antibiotics, hormonal drugs, diuretics, antihypertensive drugs, multivitamins and dietary supplements.
It is also important to prepare properly on the day of the test. It is better to follow these recommendations :
- avoid physical activity, sit quietly for 15 minutes before donating blood;
- try not to be nervous;
- do not smoke on the day of the test;
- You can drink water, even immediately before donating blood, as it does not affect cholesterol levels.
It is recommended to donate blood while sitting; if the patient stands, the cholesterol level will increase, and if the patient is lying down, it will decrease.
How is cholesterol in the blood determined and measured?
Cholesterol is part of a protein-fat compound called lipoproteins. It is present in every cell, in an unchanged pure form. And in the blood serum it is in a modified – ethereal state. The blood obtained during the tests is placed in a centrifuge so that the red blood cells settle faster.
The light-colored liquid that forms above the sediment is whey. It is from this that cholesterol levels are determined. Next, a chemical reaction occurs between cholesterol and a mixture of acids, which results in the formation of a brown or bluish substance.
Typically laboratories use the enzymatic method. Its essence is as follows: the ester compound of cholesterol is affected with the help of a certain enzyme. Next, a special dye is added.
There are also other methods. For example, a technique for the deposition process. There is also a technique based on photometry.
Photometry is the process of color comparison. There is a set norm in which the required amount of cholesterol is found . This normalized connection has a certain connotation.
The shade obtained as a result of testing is compared with the norm. This is done using a special apparatus. This apparatus is called a photoelectric calorimeter.
Another method is called nephelometry. He compares not the color, but the degree of turbidity. When using it, there are also standardized indicators that are compared with the data obtained during the study. All this happens thanks to a certain device. It is called a nephelometer.
The amount of cholesterol in the test sample is calculated automatically by the analyzers. Then the result is displayed.
Very small units are used to indicate results and are expressed in milligrams or milliliters. In the printout of the tests, the patient sees the amount of cholesterol expressed in millimoles per liter. This means what molecular weight of cholesterol is dissolved in a liter of blood. This standard is generally accepted throughout the world.
Designation of cholesterol in a biochemical blood test
People who are at risk of developing numerous diseases against the background of elevated levels need to know the designations of cholesterol in the test results. This will allow you to better navigate the course and course of your own illness, and will also contribute to additional control over the cholesterol level in the blood.
Explanation of meanings
By donating blood for a comprehensive lipid profile, the patient can get results with the following indicators:
- Chol or TC is an abbreviation for total cholesterol. As this indicator increases, the risk of developing atherosclerosis and other serious diseases increases.
- TRIG or TG is a designation for triglycerides. Resynthesis of the fat breakdown product forms triglycerides, which then enter the bloodstream.
- HDL – used to refer to high-density lipoprotein (HDL). This component of cholesterol transports its excess to the liver, from where it is then utilized. This type of cholesterol is aimed at preventing atherosclerosis.
- VLDL is the name given to very low density lipoproteins (VLDL). This type is produced by the liver and then enters the general bloodstream, gradually releasing fatty acids and cholesterol under the influence of vascular lipoprotein lipase, while lipids are converted into low-density lipids. It has been proven that this species provokes the formation of atherosclerosis.
- LDL – low density lipoproteins (LDL). They are formed in combination with VLDL as a result of a decrease in the concentration of fats. Provoke the development of atherosclerosis.
- IA – this abbreviation stands for atherogenic coefficient. It indicates the ratio of atherogenic and non-atherogenic fractions of lipoproteins. Its excessive values also lead to the development of atherosclerosis.
The standards for all these values are presented in the following table:
| Index | Lipid level (mmol/l) | ||
| desirable | border | pathological | |
| Total cholesterol (TC) | Less than 5.26 | 5,26-6,5 | More than 6.5 |
| Triglycerides | Less than 2.0 | 2,0-2,5 | More than 2.5 |
| LDL cholesterol | Less than 3.5 | 3,5-4,5 | More than 4.5 |
| HDL cholesterol | More than 1.0 | 0,9-1,0 | Less than 0.9 |
| Total cholesterol/LDL cholesterol – atherogenic coefficient | Less than 5.0 | 5,0-6,0 | More than 6.0 |
What do deviations from the norm indicate?
If the Chol level does not correspond to generally accepted parameters, then a lipid profile is required.
Factors that provoke an increase in indicators are the following:
- Diabetes;
- Liver and kidney pathologies;
- Gastrointestinal problems;
- Excessive overeating of fried and fatty foods;
- Heart attack;
- Hepatitis;
- Pancreatitis;
- Stroke;
- Cardiac ischemia.
Low cholesterol is caused by:
- Stress;
- Fasting diets;
- Anemia of various origins;
- Pathologies in lipid metabolism.
Triglycerides increase when Chol levels are elevated, but care must be taken because, for example, when using contraceptives, the same increase occurs.
What to do in case of deviations
If the indicators change slightly, then do not panic. All that needs to be done at this stage is to adjust your lifestyle.
To do this, the following factors need to be changed:
- First of all, you need to give up bad habits - alcohol and smoking.
- It is necessary to establish the correct diet, as well as adjust the diet itself. In case of increased indicators, it is necessary to sharply reduce the consumption of meat and seafood (to one dish per week), eliminate the consumption of fatty foods, sweets and flour, diversify the diet with all kinds of vegetables, fruits and the consumption of low-fat fermented milk products.
- Change your lifestyle by adding as much movement as possible. Walking is highly recommended. With the help of modern gadgets that count steps, this will be easier and more interesting. The number of steps taken should be about ten thousand, preferably if the walk takes place in the fresh air. Daily exercise also has high rates of positive dynamics in lowering cholesterol levels. You need to activate your day to the maximum, and then go to bed on time, since healthy sleep is also an integral part of the wellness program.
A month later, after adjusting your diet and lifestyle, you must take a repeat test.
Rules for conducting research
Cholesterol is produced by the liver at night. In the morning, with the help of bile, it is delivered to the intestines in order to ensure the normal digestion process. Therefore, its maximum concentration is observed in the morning. Because of this, the analysis is carried out in the morning on an empty stomach.
The patient, before testing, must follow all the doctor’s recommendations, which were detailed above.
The test results depend on the patient's responsibility. They will be correct if the patient has prepared correctly. Failure to follow the rules may lead to incorrect results. This will lead to incorrect treatment.
Research result: norm and pathology
Cholesterol levels vary depending on:
- Gender;
- Age;
- Testing method.
Considering these parameters, you can see the normal indicators in the following table:
The second table shows the norms for detailed analysis. This analysis gives a more complete picture, since it reflects not only the level of total cholesterol, but also all its fractions.
The third table gives the value of cholesterol standards, taking into account age indicators. At different periods of time, normative data change, since the amount of cholesterol increases with age.
In men, cholesterol increases throughout life. In women, cholesterol levels begin to rise after menopause.
Both overestimated and underestimated indicators are considered deviations from the norm.
Factors that provoke inflated values are divided into:
- Physiological. These factors include:
- Pregnancy;
- Excessive fatness;
- Elderly age;
- Genetic predisposition;
- Low physical activity;
- Overeating fatty, fried foods;
- Frequent consumption of fast food;
- Taking certain medications.
- Pathological. Pathologies include:
- Diabetes;
- Pancreatitis;
- Alcoholism;
- Pituitary disorders;
- Diseases of the endocrine system;
- Obesity.
Low scores are also a deviation. What causes the underestimated values?
This:
- Tuberculosis;
- Infectious diseases;
- Vitamin deficiency;
- Oncological diseases;
- Frequent diets based on fasting;
- Central cachexia.
After assessing the results, if there are obvious deviations from the norm, the doctor makes nutritional adjustments. Medications are never prescribed right away, because, often, it is enough to change your lifestyle to level out the indicators.
Independent interpretation of results
Within a couple of hours or the next day you will receive a form with the results, which you can decipher yourself or contact your doctor. As a rule, all indicators are written in Russian, and to the right of the results are the norms, which may vary slightly depending on the clinic’s data. The standard unit of measurement is mmol/l. Below is an example of a blank form for the results of a biochemical analysis.
As a rule, cholesterol in a biochemical blood test is designated as “Total cholesterol” or in Russian letters “CS”. Other designations do not cause any difficulties. However, very rarely you may come across symbols written in English or Latin, which causes difficulties for the average person to decipher. This is due to the research being carried out in a semi-automatic mode, that is, the form is filled out with foreign-made analyzers, the laboratory worker only provides blood samples for research.
So, you can often see in the results forms:
- Chol or (cholesterol) – total cholesterol;
- HDL or (high density lipoprotein) - high density lipoproteins;
- LDL or (low density lipoprotein) - low density lipoproteins.
In general, a biochemical blood test is a comprehensive diagnosis of its composition for the content of biological and chemical substances, the main of which are proteins, fats, carbohydrates, triglycerides, lipids, etc. Directly in the form of the results of the analysis for cholesterol levels, to complete the picture, in addition to total cholesterol, the concentration of HDL - its least atherogenic fractions and the concentration of LDL - its most atherogenic fractions are indicated.
Total cholesterol
The total level of cholesterol in the blood implies the total content of all its fractions, which have different levels of atherogenicity, that is, the ability to settle on the walls of blood vessels. Normally, its level is about 3 mmol/l; values above 4 mmol/l are considered a disorder requiring treatment. However, total cholesterol levels strongly depend on age; closer to 50 years, a level of 5 mmol/l is considered normal. Below is a table of the average total cholesterol level according to a person’s age.
When the level of total cholesterol deviates from the norm, the risk of developing atherosclerosis increases significantly. When there is an excess of a vital component, it settles on the walls of blood vessels and forms raised cholesterol plaques that interfere with normal blood flow. The higher the total cholesterol level, the faster this process occurs, therefore, in case of a significant deviation from the norm, the patient requires immediate comprehensive treatment.
HDL
High-density lipoproteins, or the so-called “good cholesterol,” practically do not settle on the walls of blood vessels, which means they do not increase the risk of developing atherosclerosis and its consequences. In addition, they promote the breakdown and removal of saturated fats from the body. Values within 0.9-2 mmol/l are considered normal. But again, their concentration depends on age.
When HDL concentrations are lower than 0.9 mmol/l, the risk of developing cardiovascular diseases significantly increases. To increase high-density lipoprotein levels, the patient is prescribed policosanol. Today, fibrates are extremely effective for these purposes.
LDL
Low-density lipoproteins or “bad cholesterol” - they, along with very low-density lipoproteins, at elevated concentrations, settle on the walls of blood vessels, over time forming cholesterol plaques that interfere with normal blood circulation. Normally, their level should not exceed 3.5 mmol/l.
A slight excess of the LDL standard by 1-1.5 mmol/l can be reduced with the help of a well-designed hypocholesterol diet. For more serious deviations, the patient requires exclusively comprehensive therapy, which also includes taking statins, maintaining a normal regimen (work/rest), and light physical activity.
In general, these are just general indicators that allow the doctor to quickly determine the patient’s blood condition. If abnormalities are detected, to determine a more accurate picture, the doctor analyzes the entire lipid spectrum, which contains many other characteristics of the blood composition. We will talk about it in more detail a little later.
Repeated cholesterol level determination
If the patient has deviations from the norm, the doctor prescribes a special diet that excludes certain foods that cause an increase or decrease in cholesterol levels.
Next, the doctor recommends changing your lifestyle. Physical therapy is prescribed, long walks in the fresh air or visits to the pool are recommended.
Then, two months later, a repeat analysis is scheduled. If the indicators change, approaching the norm, then the patient is advised to continue diet and exercise. If not, additional drug therapy is prescribed. After this stage, after 6-8 weeks, the analysis is scheduled again.
Dynamics of HDL and LDL are indicators of treatment effectiveness. Based on the results of the analysis, the doctor assesses the status of cholesterol levels and either leaves the treatment plan unchanged or changes it.
Which doctor should I contact?
An excess of cholesterol and low molecular weight lipoproteins in the blood is treated at the first stage by a therapist, who refers it for laboratory diagnostics.
If the cholesterol level, according to test results, is not elevated and without a predominance of low molecular weight lipoproteins, then the situation can be corrected with an anti-cholesterol diet, which will be prescribed by a nutritionist.
If atherosclerosis has already manifested itself in the cardiac organ or bloodstream system, then a cardiologist should treat this pathology for cardiac pathologies. A neurologist treats damage to cerebral vessels by lipoproteins, and a vascular surgeon deals with atherosclerosis of the lower extremities.
Where can I get the analysis done?
Since the method of conducting a cholesterol test is simple, it can be done in a regular laboratory at the clinic where the patient is registered. The doctor writes out an appointment for the test, warning that it is carried out on an empty stomach.
The doctor also gives all the necessary recommendations that must be followed before the blood sampling procedure. Next, the patient donates blood from a vein, and the next day he can receive test results.
Sometimes some patients are very distrustful, so they turn to private laboratories or diagnostic centers. This option is also possible.
You just need to know that sometimes the digital values do not match. This does not come from the level of accuracy of the devices, but from the difference in methods. Thus, private laboratories often indicate their standards in brackets.
This is done for the convenience of the doctor. Because this makes it easier to verify and analyze test results.
Test results depend on:
- Data analyzer;
- Laboratory assistant experience;
- Compliance with the rules of preparation for analysis;
- Compliance with the expiration date of chemical reagents;
- The correctness of the test technology.
The most important point is the third. Compliance with the rules for preparing for analysis is very important.
Decoding indicators
There are also age-specific norms for the concentration of cholesterol molecules. For example, in newborns the normal value is 3.5 mmol/l, and in adolescent children this figure increases to 5 mmol/liter.
Such fluctuations are due to the growth of the body, as mentioned in a scientific publication in the journal “Atherosclerosis and Dyslipidemia.” Deciphering in adults often gives errors, since the content of cholesterol molecules, lipoproteins of different densities and triglycerides in their blood depends on their lifestyle, hormonal characteristics and age category. For example, in women, LDL and VLDL can increase during menstruation, pregnancy and breastfeeding. The normal value for them is 3.5, while for males it is 4.8 mmol/l.
Functions of cholesterol in the body
Cholesterol is a fatty alcohol, a precursor to steroid hormones. Its functions in the body are essential. The body needs it. Recently, the attention of doctors has been focused on the problem of the development of atherosclerosis.
Cholesterol plays a major role in this matter. By maintaining its normal level, we prevent the development of this dangerous disease.
In addition to its negative effects, cholesterol also solves many problems. Its main functions are as follows:
- It is involved in the creation of cells, regulates their permeability, maintains their normal shape and membrane function. By stabilizing their functioning, cholesterol prevents the destructive effects of free radicals.
- Acts as a transport for useful elements. For example, it supplies oxygen to the brain. It also transports harmful substances. It collects its “harmful” fraction throughout the body, transporting it to the liver for further processing and disposal.
- Supports normal hormonal levels. Cholesterol is involved in the production of important sex hormones such as estrogen, testosterone and cortisol.
- Supports the normal functioning of the gastrointestinal tract, as it participates in the synthesis of bile.
- It is necessary during the gestation period, as it participates in the creation of new fetal cells and supports their normal functioning. Mother's milk, rich in cholesterol, helps her baby grow healthy and strong.
- It affects mental abilities, as it participates in the functioning of the brain, providing it with normal oxygen and nutrients.
- Cholesterol has been proven to prevent the onset of Alzheimer's disease.
Reference values for children
You can also read: Flaxseed oil for high cholesterol
Cholesterol standards are graded depending on age. The accepted values for children are lower than for adult patients, since in a child’s body:
- the reproductive and reproductive systems are not fully formed;
- the rate of metabolism of fat and sugar differs;
- the process of processing and assimilation of food is different;
- hormonal levels are unstable.
The amount of endogenous and exogenous cholesterol increases in proportion to the growth and development of the child. Accordingly, the norms of its content in the blood change.
Normal children's indicators
| Age | Up to 30 days | Up to a year | Up to 12 years | Up to 16 years old |
| mmol/l | 1,6 – 3 | 1,8 – 3,7 | 3,7 – 4,5 | 3,8 – 5,0 |
Cholesterol structure
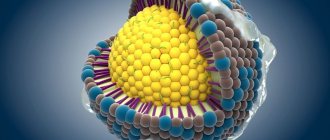
The human body contains from 140 to 350 grams of cholesterol. Ten percent of this component circulates in the blood, the remaining eighty is in the tissues. Cholesterol is insoluble in water, but soluble in fat. Lipoproteins carry cholesterol throughout the body.
The density of different levels determines the structure of cholesterol in the body. All cholesterol is divided into the following fractions:
- HDL - high-density lipoprotein - is “good” cholesterol, which performs many positive functions, its concentration in the body is 20-24%;
- VLDL - very low density lipoproteins - is “bad” cholesterol, which increases the risk of developing sclerotic plaques, is found in 9-10% of the body;
- LDL - low-density lipoproteins - is also “bad” cholesterol, found in 70%.
The source of LDL is animal fats. This faction is characterized by negative nicknames - bad, no good, harmful. But this type of cholesterol is necessary for the body.
It provides the body's cells with the necessary nutrition, helping them absorb vitamins. This type also neutralizes toxins. But excessive concentration of this fraction leads to the development of atherosclerotic plaques.
The consequences of this negative process can be:
- Ischemic attacks;
- Heart attack;
- Stroke;
- Arterial diseases.
The structure of HDL differs from the structure of LDL. They have the exact opposite effect. These lipoproteins collect all residual cholesterol and transport it to the liver to be further processed and removed from the body. This reduces the risk of developing atherosclerosis.
Why is cholesterol dangerous?
Although cholesterol has its positive sides, it can be harmful.
Its negative impact on the body is manifested in the following pathologies:
- Provokes cholelithiasis. With an increased concentration in the gallbladder, cholesterol forms balls of a solid structure that can block the bile ducts and prevent the normal passage of bile. Symptoms of cholecystitis are marked by sharp pain in the right side, in the hypochondrium. The only way to get rid of cholesterol deposits in the gallbladder is through surgery.
- Atherosclerosis. This is the main negative property of cholesterol being deposited on the arteries in the form of atherosclerotic plaques. This ability is present in low molecular weight and very low molecular weight lipoproteins. High molecular weight lipoproteins are trying to resist them, but they are in the minority. High molecular weight lipoproteins occupy only (1/3 of the total volume of total cholesterol in the blood).
Cholelithiasis
How and why cholesterol is produced in the liver
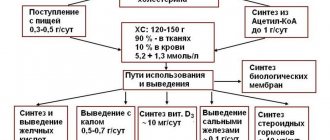
The human body is aimed at quickly restoring and maintaining health. The body is like a complex machine. Millions of processes take place in it every day. From the general information of the article, it is clear that 80 percent of cholesterol is generated by our liver, the remaining 20 we get from food.
It would seem that if you can get everything through food, then why does the liver need additional stress?
The fact is that staple foods contain low-density cholesterol (LDL), and excess amounts of it lead to the formation of sclerotic plaques. Our liver is on guard.
In order to prevent the development of atherosclerosis, it has to synthesize another fraction of lipoproteins. These are high density lipoproteins (HDL). They are needed to prevent atherosclerotic plaques.
With the help of HDL, the liver filters out the “bad” cholesterol and removes it from the body in the form of bile. The pathway of cholesterol biosynthesis in the body is very complex. It takes place in several stages.
Diagnostics
In order to check the level of cholesterol in your blood, you need to undergo a laboratory test:
- A blood test for cholesterol (total) shows the total cholesterol index. It can be taken even after eating,
- Lipoprotein biochemical analysis is a more detailed study of the composition of the blood for the presence in it of: triglycerides, HDL and LDL,
- Direct analysis of the level of low molecular weight lipoproteins LDL. This test can be taken even on a full stomach.
How the body uses the substance
Synthesized cholesterol performs many positive functions in the body: it produces steroid hormones, participates in the production of vitamin D, and plays the role of transport, as it circulates in the circulatory system throughout the body.
Our skin contains a lot of cholesterol, since under the influence of ultraviolet radiation vitamin D is produced from cholesterol. This vitamin is responsible for the body’s absorption of calcium, which is very important for bones.
The molecular functions of cholesterol are in the transport process. Nutrients, oxygen, and certain groups of coenzymes are not able to penetrate tissues on their own. Cholesterol helps them “get” to their “destination.”
Cholesterol production is a complex, energy-consuming process that the human liver performs every day.